Translate this page into:
Miliary gout: A rare case report from North India

*Corresponding author: Ranveer Singh Jadon, Department of Medicine, All India Institute of Medical Sciences, New Delhi, India. dr.ranveerjadon@yahoo.co.in
-
Received: ,
Accepted: ,
How to cite this article: Swarnkar B, Goel A, Sonai MK, Jadon RS, Khandpur S, Yadav R. Miliary gout: A rare case report from North India. CosmoDerma. 2024;4:109. doi: 10.25259/CSDM_86_2024
Dear Sir,
The atypical presentations of gout include miliary, bullous, papular, ulcerative, and verrucous.[1,2] Miliary gout presents as “milia-like” papules over the body. Herewith, we report a rare case of miliary gout to bring this to the notice of dermatologists and physicians for the early diagnosis and treatment of gout.
A 54-year-old man presented to the Department of Medicine with cardiogenic shock. He was a known case of rheumatic heart disease. A dermatology opinion was taken for cutaneous lesions.
There was a history suggestive of psoriasis for the past 7–10 years for which he used to apply topical steroid on and off. He had a history of intermittent pain over multiple joints including joints of the hands, wrists, elbows, knees, and ankle joints for the past two years. The pain was asymmetrical and was not associated with morning stiffness or history suggestive of enthesitis. Some of the affected joints showed erythematous swelling with mild or no associated pain. The patient did not get evaluated for the same and took over-the-counter analgesics with temporary relief. He complained of asymptomatic raised hard skin lesions over the body for the past one year. He was an occasional alcohol user. The patient had a body mass index of 24.9 kg/m2, and on mucocutaneous examination, there were multiple hard, yellowish-white discrete, non-tender, papules over normal to erythematous appearing skin over bilateral shins [Figure 1], forearms, palms, and trunk. There was erythematous swelling over the second right metacarpophalangeal joint with evidence of yellowish-white nodules inside it [Figure 2]. Based on history and examination, differentials of miliary calcinosis cutis and miliary gout were kept. Punch biopsy from shin papule showed multiple nodular deposits of eosinophilic fibrillar to homogenous amorphous gouty deposits in the dermis surrounded by a palisade of histiocytes and histiocytic giant cells, characteristic of gouty deposits [Figures 3 and 4]. The biochemical analysis revealed a high serum uric acid level of 12.9 mg/dL, anemia of chronic disease, deranged kidney function test (urea 82 mg%, creatinine 2.1 mg%), high C-reactive protein (21.7 mg/dL), raised rheumatoid factor (64 IU/mL), and negative anti-cyclic citrullinated peptide (anti-CCP) antibody. Serum calcium, phosphate, and parathyroid hormone were normal. X-ray of the joints revealed juxtaarticular osteopenia. Based on the morphology of the cutaneous lesions, high serum uric acid level, and histopathology, a final diagnosis of miliary gout was made and the patient was advised to avoid alcohol, a diet low in meat, and start febuxostat 40 mg once daily. However, within a few days, the patient died due to cardiac failure.
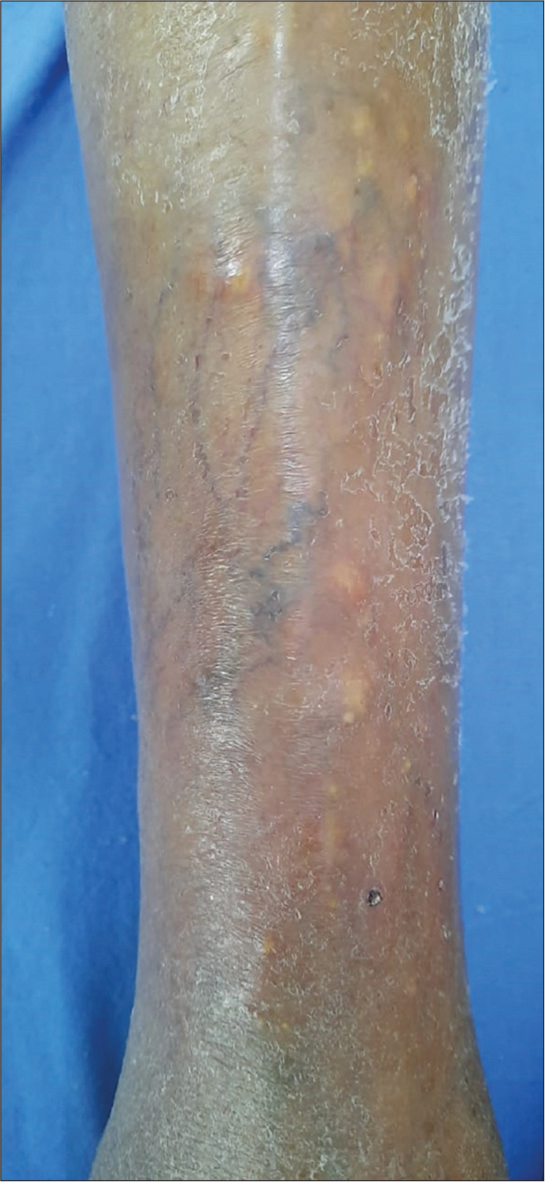
- Multiple hard, yellowish-white discrete, non-tender, and papules over normal to erythematous appearing skin over shin.
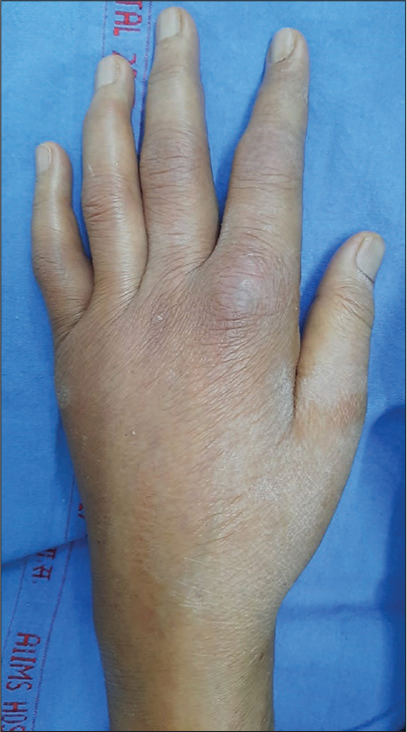
- Erythematous swelling over second right MCP joint with yellowish-white nodules inside it (nodules are not clear in picture).
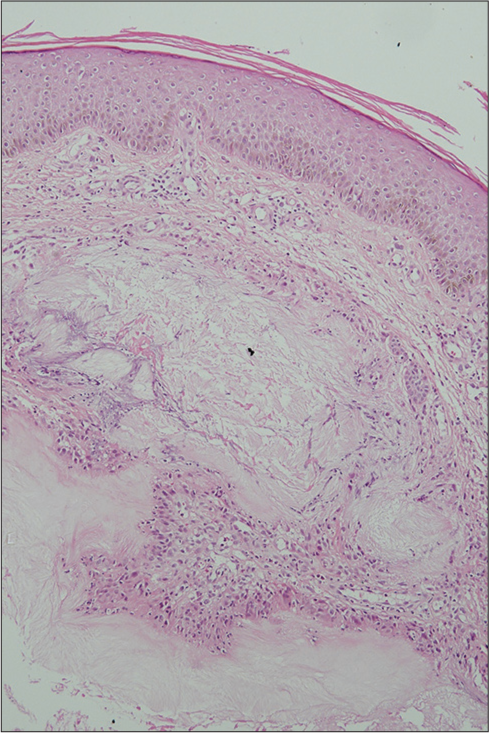
- Eosinophilic amorphous gouty deposits with surrounding giant cells and lymphoid proliferation in the dermis (× 10, H and E Stain).
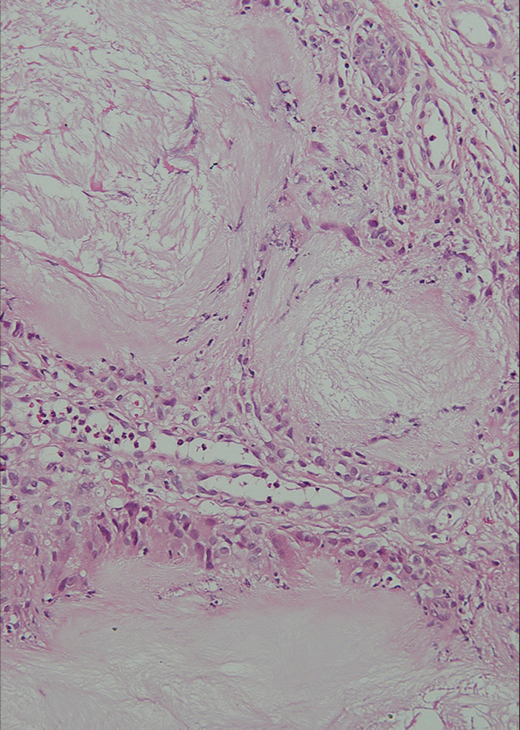
- Eosinophilic amorphous gouty deposits with surrounding giant cells and lymphoid proliferation in the dermis (× 20, H and E Stain).
Gout is a common systemic metabolic disorder caused by abnormal uric acid metabolism. Untreated gouty arthritis can result in intra-dermal and deeper deposition of monosodium urate (MSU) crystals in the fat usually over the peri-articular area, cartilage or over normal skin resulting in chronic cutaneous tophaceous gout.[2] Individuals with long-duration gouty arthritis, psoriasis, renal insufficiency, and lack of consistent use of urate-lowering therapy (as in our case) are at high risk of intradermal tophi formation. Psoriasis predisposes to hyperuricemia by activating Th1 and Th17 pathways which play a role in the pathogenesis of gout. This common cytokine pathway might point toward the association between gout and psoriasis. In addition, an increased keratinocyte turnover rate leads to increased purine metabolites causing increased serum uric acid levels. Genetic factors and metabolic syndrome also link psoriasis with gout.[3,4]
A miliarial gout is a rare form of chronic tophaceous gout, which presents as “milia-like” papules containing white, cream, or yellow-colored material on an erythematous base on the skin over various body parts.[1] The pathogenesis of intra-dermal tophaceous gout is yet to be elucidated, but it has been hypothesized that the rate of formation of urate crystals exceeds the handling capability of macrophages or probably the failure of tissue macrophages to differentiate to an endpoint, which does not produce a proinflammatory response to MSU crystal uptake.
There are few reports of miliary gout worldwide [Table 1]. Diagnosis of cutaneous tophaceous gout can be made by seeing amorphous crystalline material with surrounding granulomatous inflammation in histopathology and negatively birefringent needle-like crystals on polarized microscopy. X-ray of joints in gouty arthritis shows juxtaarticular erosions with sclerotic margins and overhanging edges with normal periarticular bone density and preserved joint space until the disease has reached late stage but it can be normal (as seen in our patient) as mentioned in report by Aguayo et al.[2] The main differential is rheumatoid arthritis with calcinosis cutis. Both can be differentiated by serological and biochemical investigations. In our patient, rheumatoid arthritis with calcinosis cutis was ruled out by normal biochemical profile, along with negative anti-CCP level and skin histopathology findings. Others include pseudogout, oxalosis, and rheumatoid nodules. They are tabulated in Table 2. The treatment of chronic gout aims to prevent gout progression and flares, eliminate any MSU deposits, and prevent further tophus formation. Xanthine oxidase inhibitors (febuxostat and allopurinol) are the first-line treatment options followed by uricosuric agents (probenecid). This case is interesting given a rare cutaneous manifestation of chronic gout, that is, miliary gout. This also intends to sensitize physicians and dermatologists about this rare entity for its early diagnosis and management to prevent catastrophic outcomes such as renal failure, cardiac failure, and death.
| S. No. | Year | Author | Cutaneous manifestations | X-ray joints | Serum uric acid | Treatment given |
|---|---|---|---|---|---|---|
| 1. | 2007 | Shukla et al.[1] | Papules over forearms and shins | – | 13243.23 mg/dL | Allopurinol and colchicine |
| 2. | 2013 | Aguayo et al.[2] | Papules over left shin with underlying gouty panniculitis | Normal | 11.4 mg/dL (2.0–7.0 mg/dL) | Allopurinol |
| 3. | 2013 | Lo et al.[5] | Yellow nodules over forearms, shoulders and upper torso and tophi over finger joints, hands | Features consistent with gouty arthritis | 55.176 mg/dL | Colchicine and prednisone followed by allopurinol |
| 4. | 2014 | Mireku et al.[6] | Papules over MCP joints of his hands, knees, abdomen, extensor forearms and thighs | – | Normal | – |
| 5. | 2015 | Kirchhof et al.[7] | Papules and nodules thighs and legs | – | 12810.798 mg/dL | Allopurinol and colchicine |
| 6. | 2016 | Hung et al.[8] | Papules and plaques over elbows, knees, and upper arms | – | 10.7mg/dL (2.3–7.0 mg/dL) | – |
| 7. | 2017 | Gianfaldoni et al.[9] | Papules and nodules over b/l elbows | Normal | 15.0 mg/dL | Allopurinol |
| 8. | 2018 | Sadovici-Bobeica et al.[10] | White papules with carpal tunnel syndrome | - | 6.1 mg/dL | – |
| 9. | 2018 | Kim et al.[11] | Papules over pretibial areas with tophaceous nodules over periarticular areas | - | 11.4 mg/dL | – |
| 10. | 2019 | Pradhan et al.[12] | Periarticular subcutaneous tophi, disseminated intradermal form, ulcerative, and miliarial tophi (palms, tips of fingers) | There was destruction of bilateral MTP joints and first IP joint of right foot. There were multiple juxta-articular joint erosions with sclerosis and overhanging margin | 16.2 mg/dL | Allopurinol |
| 11. | 2020 | Parlindungan et al.[13] | Nodules and ulcers over Trunk and extremities |
– | 11.5 mg/dL (3.4–7.0 mg/dL) | Steroid, colchicine and allopurinol |
MCP: Metacarpophalangeal, MTP: Metatarsophalangeal, IP: Interphalangeal
| S.No | Differential | Classical features |
|---|---|---|
| 1. | Calcinosis cutis with Rheumatoid arthritis | Positive anti-CCP antibody. Destructive symmetric peripheral polyarthritis with skin nodules. Histopathology of calcinosis cutis shows amorphous basophilic deposits in the dermis with surrounding foreign giant cell infiltrate and positive staining with Von Kossa stain |
| 2. | Pseudogout | Monoarticular arthritis. It shows basophilic amorphous calcium deposits with rhomboid-shaped crystals surrounded by chronic inflammatory infiltrate in skin tissue histology |
| 3. | Oxalosis | Symmetric polyarticular arthritis, nephrolithiasis, and skin nodules. Skin biopsy shows yellow-brown rhomboid crystals surrounded by histiocytes in the dermis and subcutis. Multicolored, birefringent crystals are observed in polarized microscopy |
| 4. | Rheumatoid nodules with Rheumatoid arthritis | Destructive symmetric peripheral polyarthritis with skin nodules. Positive anti-CCP antibody. Histology of skin nodules shows red granuloma with a central area of necrotic collagen surrounded by eosinophilic fibrin deposition, which in turn is surrounded by palisading chronic inflammatory cells. Around this layer, there is vascular connective tissue rich in plasma cells |
CCP: Cyclic citrullinated peptide
Acknowledgement
Dr. Sindhuja Tekumalla for help with the clinical diagnosis and evaluation of the patient.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Unilateral milia-type intradermal tophi associated with underlying urate subcutaneous deposition: An uncommon cutaneous presentation of gout. Clin Exp Dermatol. 2013;38:622-5.
- [CrossRef] [PubMed] [Google Scholar]
- The risk of gout in patients with psoriasis: A population-based cohort study in Taiwan. Clin Epidemiol. 2022;14:265-73.
- [CrossRef] [PubMed] [Google Scholar]
- Chronic tophaceous gout in patients with psoriasis. An Bras Dermatol. 2017;92:104-6.
- [CrossRef] [PubMed] [Google Scholar]
- "Golden Kernels within the skin": Disseminated cutaneous gout. BMJ Case Rep. 2013;2013:bcr2013009735.
- [CrossRef] [PubMed] [Google Scholar]
- Miliarial gout: A rare clinical presentation. J Am Acad Dermatol. 2014;71:e17-8.
- [CrossRef] [PubMed] [Google Scholar]
- Multiple cutaneous creamy papules and nodules: A case of miliarial gout. J Cutan Med Surg. 2015;19:317-9.
- [CrossRef] [PubMed] [Google Scholar]
- Miliarial gout: A rare presentation of extensive cutaneous tophi. QJM Int J Med. 2016;109:811-2.
- [CrossRef] [PubMed] [Google Scholar]
- Asymptomatic papules and subcutaneous nodules as first sign of gout. Open Access Maced J Med Sci. 2017;5:511-4.
- [CrossRef] [PubMed] [Google Scholar]
- Chronic miliarial gout associated with carpal tunnel syndrome: A very rare clinical presentation. Eur J Case Rep Intern Med. 2018;5:000926.
- [CrossRef] [PubMed] [Google Scholar]
- Unusual milia-type intradermal tophi in a patient with gout. Korean J Intern Med. 2020;35:736-7.
- [CrossRef] [PubMed] [Google Scholar]
- Atypical cutaneous presentation of chronic tophaceous gout: A case report. Indian Dermatol Online J. 2020;11:235.
- [CrossRef] [PubMed] [Google Scholar]
- Disseminated cutaneous tophi in a patient with chronic tophaceous gout and renal impairment: A case report of a rare manifestation of gout. Am J Case Rep. 2020;21:e919349.
- [CrossRef] [PubMed] [Google Scholar]





