Translate this page into:
Linear porokeratosis and the rationale of combining calcipotriol with 5-fluorouracil

*Corresponding author: Jagjeet Kaur Sethi, Department of Dermatology, Aesthetics and Lasers, Hope Clinic, Shillong, Meghalaya, India. jagjeetsethi@hotmail.com
-
Received: ,
Accepted: ,
How to cite this article: Syiemlieh A, Sethi JK. Linear porokeratosis and the rationale of combining calcipotriol with 5-fluorouracil. CosmoDerma. 2025;5:14. doi: 10.25259/CSDM_185_2024
Abstract
Linear porokeratosis is one of the rare forms of porokeratosis and is also pre-malignant in nature. The term porokeratosis is a misnomer, as it is not a disorder of the sweat gland ducts, but rather a disorder of keratinization. There is no standard of therapy for porokeratosis and many topical therapies exist such as topical retinoids; keratolytics such as salicylic acid and urea; topical vitamin D3 analogs such as calcipotriol and calcipotriene, along with the newer 2% lovastatin creams with or without 2% cholesterol cream. We report this case of linear porokeratosis since we have combined 5% 5-fluorouracil cream and 0.005% calcipotriol ointment for both clinical cure and cancer immunotherapy. Although it is a common combination used in the treatment of actinic keratosis, another premalignant dermatosis, it has been uncommonly used in porokeratosis of Mibelli and never reported to be used in linear porokeratosis.
Keywords
Calcipotriol
5-fluorouracil
Immunotherapy
Linear porokeratosis
INTRODUCTION
Porokeratosis is a disorder of keratinization first coined in 1893 by Mibelli and Respighi. The term as is now known, is a misnomer, which when translated from its Greek origins means “thickening” of pores of sweat glands.[1] We report a case of linear porokeratosis and discuss the rationale of combining calcipotriol with 5-fluorouracil (5-FU) in this case and its potential use in all the premalignant types of porokeratosis.
CASE REPORT
A 9-year-old patient presented to us at the clinic with raised dark lesions in a linear fashion along the entire length of the back of the right leg, which had been present since the patient was 6 years of age. It was asymptomatic with no itching, redness, pain, or discharge. She had already sought treatment from multiple dermatologists with no help. She had no co-morbidities. None of the family members had a similar rash, and the patient was born out of a non-consanguineous marriage. On cutaneous examination, linear hyperpigmented papules and few plaques were noted to arise from the Achilles tendon up to the mid-gluteal region sparing the natal cleft, some were flat with a hyperpigmented rim, some were more keratotic, and some had verrucous surface changes [Figure 1a-d]. Her oral and genital mucosae, nails, and hair were normal. We considered linear porokeratosis, inflammatory linear verrucous nevus, and lichen striatus as our differentials. Dermoscopy revealed multiple circular plaques having rimmed edges and hyperpigmentation under the edges [Figure 2a]. A polarised dermoscopy was done [Figure 2b] at four months as a comparison to show the reduction in scaling post treatment within some of the residual plaques. A biopsy was taken from the plaque on the Achilles tendon area which revealed “cornoid lamellae,” which are columns of parakeratotic cells invaginating through the epidermis with underlying relative hypogranulosis at multiple foci. Some dyskeratotic cells were seen. The dermis had moderately dense perivascular lymphocytic infiltrate. All these findings were consistent with porokeratosis [Figure 3 and b] Routine blood investigations revealed mild anemia with a hemoglobin level of 11.1 g/dL and a relatively normal hemogram. She was started on 5% 5-FU cream application for an hour at bedtime and 0.005% calcipotriol ointment application in the morning, over the lesions with a significant reduction in lesions in just 2 months [Figure 4]. There was only a history of mild redness on the initial days of application over the lesions and no sign of the same at the follow-up examination. She had predominantly only post-inflammatory hyperpigmentation by 4 months of treatment [Figure 5a-c] on the limb and some persistent thin plaques [Figure 5d] seen on the tendo-Achilles. The mother had been counseled on the risk of recurrence, malignant change, and the need for a regular follow-up despite lesions appearing normal.
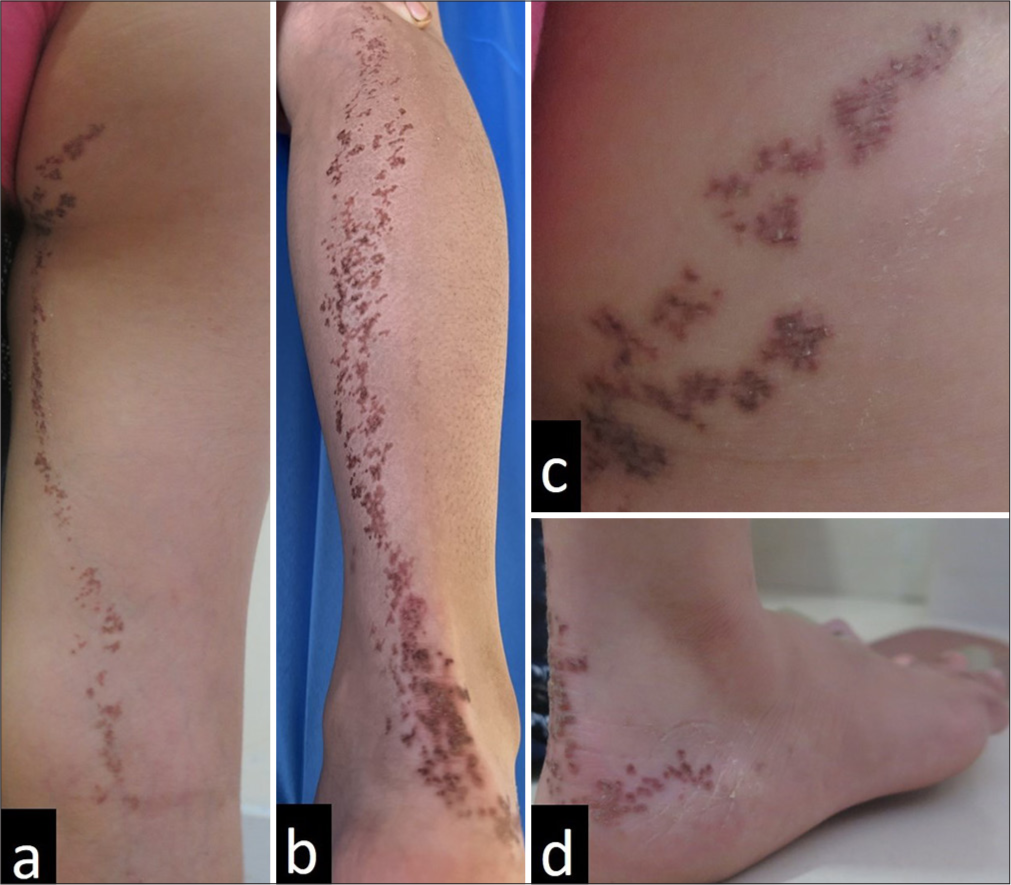
- A 9-year-old girl presented with hyperpigmented keratotic and scaly papules coalescing to form linear plaques all along the entire length of the (a,b) posterior right leg . (c) shows a close up of the plaques on the right side of buttock and (d) shows the lesions extending to the postero-lateral aspect of the right foot.
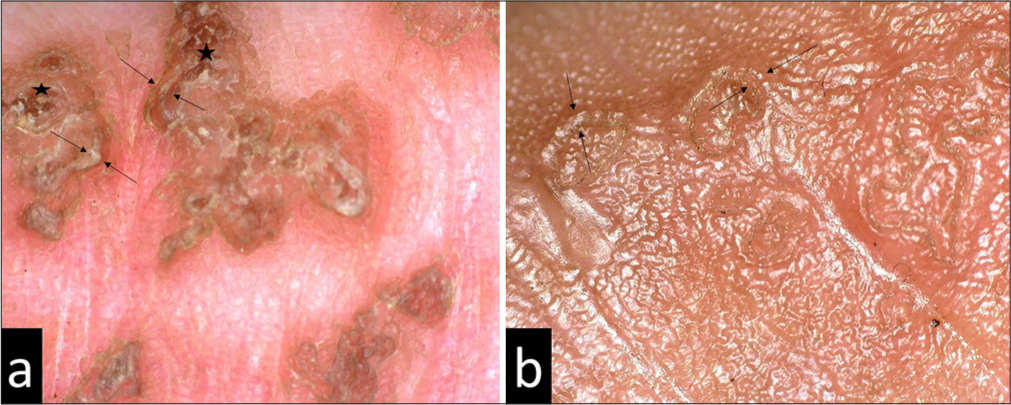
- Dermoscopy showing characteristic rimmed edge (in between arrows) and pigmentation under the keratotic rim (star). (a) Dermoscopy done at presentation (Dino-Lite Edge digital microscope, ×50, polarized). (b) Comparison Dermoscopy done after 4 months (Dino-Lite Edge digital microscope, ×70, nonpolarized).
![A biopsy of the plaque from the Achilles tendon shows multiple “cornoid lamellae,” invaginating through the epidermis (H and E, ×100) with underlying hypogranulosis at multiple foci (hematoxylin and eosin [H and E], ×400). (a and b) show a moderately dense perivascular upper dermal infiltrate, seen to be (b) lymphocytic in nature.](/content/130/2025/5/1/img/CSDM-5-14-g003.png)
- A biopsy of the plaque from the Achilles tendon shows multiple “cornoid lamellae,” invaginating through the epidermis (H and E, ×100) with underlying hypogranulosis at multiple foci (hematoxylin and eosin [H and E], ×400). (a and b) show a moderately dense perivascular upper dermal infiltrate, seen to be (b) lymphocytic in nature.

- At two months, during treatment with the 0.05% calcipotriol with 5% 5-fluorouracil combination showing significant reduction in lesions.
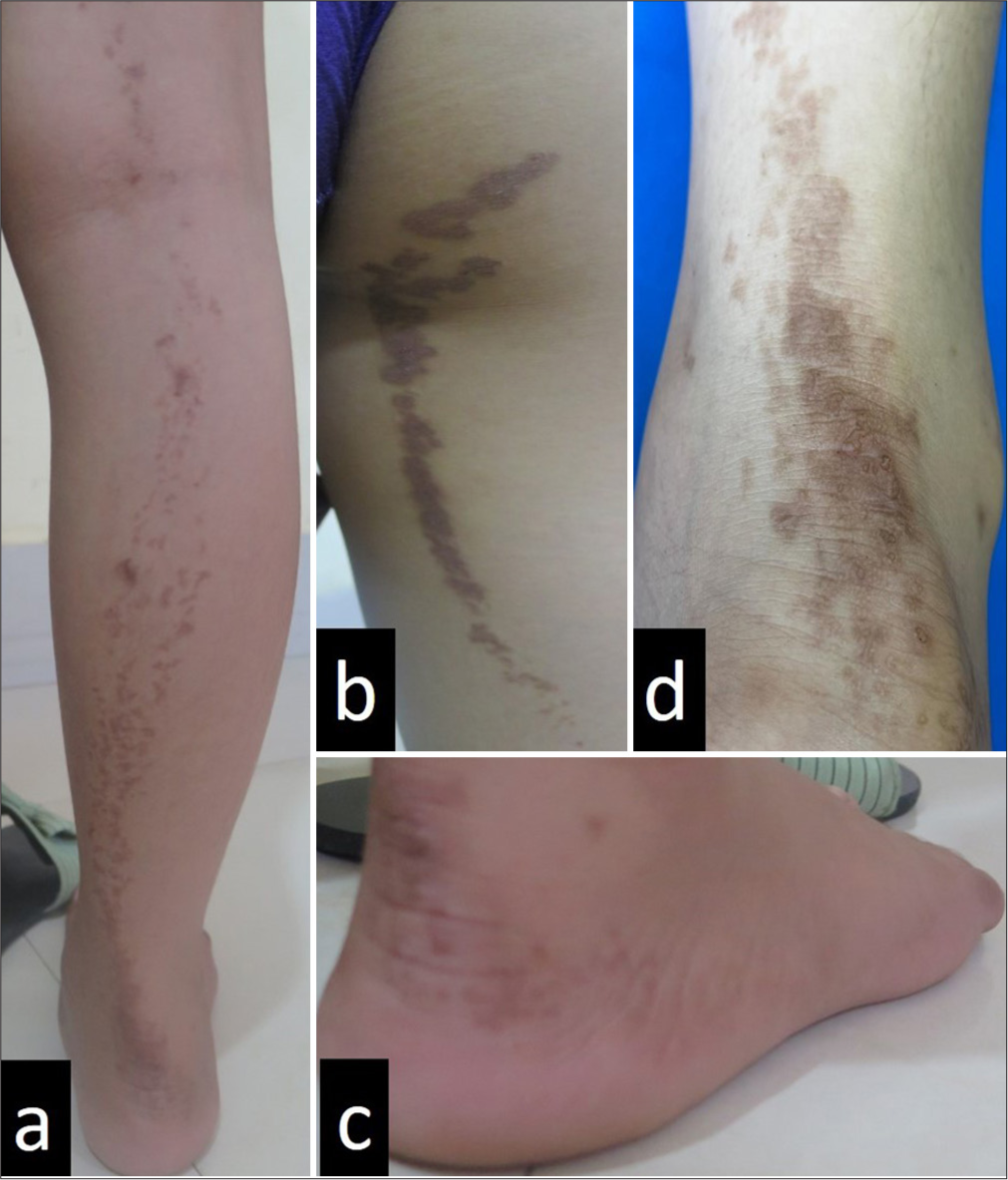
- After four months of treatment, the patient is left predominantly with (a, b and c) post-inflammatory hyperpigmentation and (d) some residual keratotic plaques over the tendo-Achilles.
DISCUSSION
Over the years, porokeratosis has been found to actually be a clonal keratinization abnormality. It may be acquired but is mostly autosomal dominant in inheritance and sometimes sporadic in nature. The risk factors for acquiring porokeratosis are prolonged ultraviolet exposure, drugs such as furosemide, benzenes, tumor necrosis factor alpha inhibitors, and infectious agents such as the human papillomavirus (HPV) virus and immunosuppressed states. It was recently postulated by Atzmony et al.[2] that linear porokeratosis is a disorder of mosaicism in genes encoding the enzymes, phosphomevalonate kinase, and mevalonate diphosphate decarboxylase involved in the mevalonate biosynthesis pathway, essential for the synthesis of compounds such as cholesterol, a component of the stratum corneum lipid matrix. This depletion in cholesterol and a buildup of unwanted metabolites due to disruption in the normal pathway results in dyskeratotic keratinocytes.
The main clinical types of porokeratosis are porokeratosis of Mibelli, disseminated superficial porokeratosis, disseminated superficial actinic porokeratosis; porokeratosis palmaris et plantaris disseminate, punctate porokeratosis, and linear porokeratosis. While others are said to be autosomal dominant, porokeratosis of Mibelli and linear porokeratosis are seen due to somatic mosaicism. The linear type of porokeratosis is the rarest form of all the types, and in itself, it may be localized, systematized, or generalized. The localized variety usually involves only a single limb following the lines of Blaschko in the extremities and a zosteriform distribution in the trunk. In the limbs, it affects the distal more than the proximal part.[3] While the systematized form is more disseminated and may be bilateral, the generalized variety affects multiple limbs and the trunk.
Up to 30% of porokeratosis patients develop skin cancer, of which squamous cell carcinoma is the most common. Bowen disease is also seen and less commonly, basal cell carcinoma. Malignant transformation usually occurs with linear porokeratosis, large and long-standing lesions as compared to other types of porokeratosis.[4]
Dermoscopy of all porokeratosis lesions reveals the same characteristic finding which is the “white track” or “keratinous striae,” which is the peripheral keratinous rim that is whitish to yellowish in color and is well defined with some evidence of linear, annular, or punctate hyperpigmentation and with linear or punctate vessels occasionally.[5] On biopsy of the porokeratotic lesions, it is yielding to biopsy from the keratotic rim as this shows the characteristic finding of the lesion which is the cornoid lamellae. The cornoid lamella is the parakeratotic invagination of the corneocytes with an overlying orthokeratotic stratum corneum. There is underlying hypogranulosis with dyskeratosis of the underlying and adjacent spinous layer keratinocytes. The dermis may show some dilated capillaries with perivascular lymphocytes.
The treatment may be medical or surgical or both, including conventional as well as the use of more novel therapies. Treatment with salicylic acid and urea as keratolytics and even topical retinoids has not shown very satisfactory results. 5% Imiquimod has been found useful in some cases and has been linked to possible HPV virus association. Topical steroids, 0.1% Tacrolimus, 5% 5-FU, and 0.005% calcipotriol have been used separately usually with varying responses. Often a combination of oral retinoids or any topical treatment, accompanied by local destruction of the lesions by cryotherapy, curettage, excision, or carbon dioxide laser are the surgical options available. The defect in the mevalonate pathway has led to recent studies finding success with topical lovastatin 2%. It has been found to be as effective alone, as the combination with 2% cholesterol as it decreases mevalonate levels and inhibits the formation of toxic metabolites.[6] We opted to combine calcipotriol and 5-FU with the rationale that has been inspired by the multitude of studies on this combination being used in pre-malignant actinic keratoses and cancer prevention immunotherapy.
5-FU is a pyrimidine analog that inhibits DNA synthesis by inhibiting the enzyme thymidylate synthase, thus blocking the conversion of deoxyuridylic acid to thymidylic acid. This leads to cellular death of proliferating cells such as cancer-causing cells. Calcipotriol being an analog of vitamin D3 acts by binding to vitamin D receptors, inhibits keratinocyte proliferation, and regulates cellular differentiation.[7] In addition, calcipotriol has been found to trigger the release of the cytokine, thymic stromal lymphopoietin (TSLP) which in turn leads to an influx of CD4 + T cells that have tumor-cell cytotoxicity and memory which gives protection in the long term.[8]
The combination of these two drugs results in many synergistic benefits. The first is an amplification of the CD4 + T cell release.[7] Second, it also induces a major histocompatibility complex (MHC) Class II and MHC Class I-related Chain B (MICB) expression on the malignant keratinocytes, which act as antigen-presenting cells and make it easier for the CD4+ cells to target the malignant cells. Third, the combination stimulates natural killer group 2, member D receptor expression on keratinocytes which binds to ligands such as MICB, causing cytotoxicity and enhanced anti-tumor effect of TSLP.[8]
In a study on skin cancer prevention immunotherapy, this combination has been found to be significantly better than 5-FU alone in suppressing skin cancer in mice.[8] Another study conducted in 2021 used 5-FU and calcipotriene for porokeratosis of Mibelli with clearance of lesion in 5 days.[9] Rosenberg et al.[10] also conducted a study on skin cancer immunotherapy with a 5-FU/calcipotriene combination and found that it prevented squamous cell cancer formation on the face and scalp within three years of treatment. It must be noted that the combination used for actinic keratosis is a 50: 50 use of 5% 5-FU cream with 0.005% calcipotriol. We have used a morning and evening application of each of the creams and asked the patient to leave on the 5-FU for only an hour as the peak effect is seen within 1 h.[7] We believe that these two factors were the reasons for the low side effect profile with our patient noting only mild erythema. Erythema is often noted post-application of 5-FU and indicates immune induction against the premalignant keratinocytes.[7] While there was absolutely no doubt of the clinical clearance by this modality, its cancer immunotherapy can only be reported with follow-up.
CONCLUSION
This case is interesting with regard to its rarity, its extensive distribution throughout the lower limb, and also to encourage the use of this combination therapy as a form of cancer prevention immunotherapy. Many treatment modalities in porokeratosis have been advocated but no standard therapy has been devised. Only two other case reports using this combination for porokeratosis of Mibelli have been published and none yet for linear porokeratosis.
Ethical approval:
Institutional Review Board approval is not required.
Declaration of patient consent:
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest:
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship:
Nil.
References
- The man behind the eponym: Vittorio Mibelli and the tale of porokeratosis. Am J Dermatopathol. 1986;11:79-83.
- [Google Scholar]
- Second-hit, postzygotic PMVK and MVD mutations in linear porokeratosis. JAMA Dermatol. 2019;155:548-55.
- [CrossRef] [PubMed] [Google Scholar]
- Zosteriform porokeratosis of Mibelli. Arch Dermatol. 1971;104:425-6.
- [CrossRef] [PubMed] [Google Scholar]
- A case of genital porokeratosis and review of literature. Indian J Dermatol. 2015;60:217.
- [Google Scholar]
- Linear porokeratosis of the foot with dermoscopic manifestations: A case report. World J Clin Cases. 2022;10:11585-9.
- [CrossRef] [PubMed] [Google Scholar]
- Bilateral linear porokeratosis treated with topical lovastatin 2% monotherapy. Cureus. 2023;15:e43657.
- [CrossRef] [PubMed] [Google Scholar]
- Calcipotriol and 5-fluorouracil combination therapy for the treatment of actinic keratosis in the clinic: A review article. Clin Drug Investig. 2024;44:733-7.
- [CrossRef] [PubMed] [Google Scholar]
- Randomized trial of calcipotriol combined with 5-fluorouracil for skin cancer precursor immunotherapy. J Clin Invest. 2017;127:106-16.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of porokeratosis of Mibelli with combined use of topical fluorouracil and calcipotriene. JAAD Case Rep. 2021;9:54-6.
- [CrossRef] [PubMed] [Google Scholar]
- Skin cancer precursor immunotherapy for squamous cell carcinoma prevention. JCI Insight. 2019;4:125476.
- [CrossRef] [PubMed] [Google Scholar]






