Translate this page into:
Glass slide—An indispensable tool for the dermatologist

*Corresponding author: Aravind Sivakumar, Department of Dermatology and STD, Jawaharlal Institute of Postgraduate Medical Education & Research, Puducherry 605006, India.aravinddermat@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sivakumar A, Thappa DM. Glass slide—An indispensable tool for the dermatologist. CosmoDerma 2022;2:27.
INTRODUCTION
Dermatology as a field has advanced in various aspects in the 21st century as new inventions and novel investigative techniques have evolved along with the inception of artificial intelligence and machine learning. However, this is a double-edged sword as older techniques of bedside skills and examination is being ignored. One such example is the glass slide which is a powerful bedside tool for the dermatologist and hence its scope is discussed below. The use of bedside clinical tests is necessary even for an experienced dermatologist for confirmation of diagnosis, especially for similar-looking lesions. These are being replaced by evolving technology and advancements in investigative procedures. However, these simple tests remain the main method of diagnostic confirmation in routine dermatological practice, especially in resource-poor settings. Here the glass slide and the uses in various settings have been discussed.
Eliciting cutaneous signs:
This is a useful tool, especially for bedside confirmation and rapid diagnosis. The following cutaneous signs can be demonstrated bedside with the help of the glass slide.
Auspitz sign: Named after Heinrich Auspitz this was first described by Daniel Turner in the 19 century. It is usually elicited using the grattage test where the superficial scales are scraped off with the help of a glass slide which reveals a shiny glistening membrane referred to as the Bulkeley’s membrane corresponding to the thinning of suprapapillary plate. On further scraping, there is the appearance of punctate bleeding spots due to the presence of dilated dermal capillaries [Figure 1]. However, these changes can be demonstrated in other conditions such as Darier’s disease and actinic keratosis. Also can be negative in the case of guttate psoriasis, pustular or erythrodermic psoriasis, rupioid variant, inverse or flexural variant, and also in case of treated cases.[1,2]
Candle and last cuticle sign: Glass slide is useful in demonstrating scaling by gentle scraping of the lesional surface when the scales are not prominent. This is most prominently seen in chronic plaque psoriasis where the scales can be easily scraped off from the surface like shaving off the candle wax referred to as the candle sign or wax spot phenomenon (Signe de la tache de bougie ).[3,4]
Besnier’s sign: Also referred to as the scratch sign or coup d’ongle sign, here the indistinct scales of the macules in tinea versicolor can be accentuated by either scratching or scraping gently with the glass slide.[5]
Brocq’s phenomenon: This sign is akin to the Auspitz sign in psoriasis which is characterized by the presence of subepidermal hemorrhage on gently scraping the lesions in lichen planus.[6]
Dermatographism: Also referred to as skin writing is a form of physical urticaria and is due to an exaggerated triple response of Lewis characterized by linear erythema and whealing. It usually can be elicited by firm stroking of the skin with the edge of the glass slide or any blunt object following which there is the appearance of linear wheals of 2 mm or more within 1-2 minutes with the episode lasting for about half an hour [Figure 2]. In the case of symptomatic dermatographism, there might be associated pruritus in addition to whealing, unlike simple dermatographism.[7]
Darier’s sign: This is a specific form of dermatographism which is elicited in cases of cutaneous mastocytosis due to the release of mast cell mediators leading to wheal formation. However, it can also be observed in other conditions such as juvenile xanthogranuloma, histiocytosis, and leukemia cutis. Occasionally in children, it can lead to systemic symptoms including nausea, diarrhea, vomiting, hypotension, and bronchospasm hence caution must be exercised before performing in them.[8]
Pseudo Darier sign: This is similar to Darier’s sign, seen in the case of congenital smooth muscle hamartoma where there is transient piloerection and induration with or without erythema, due to the neural component of the hamartoma.[8]

- Demonstration of Auspitz sign in the case of psoriasis vulgaris.
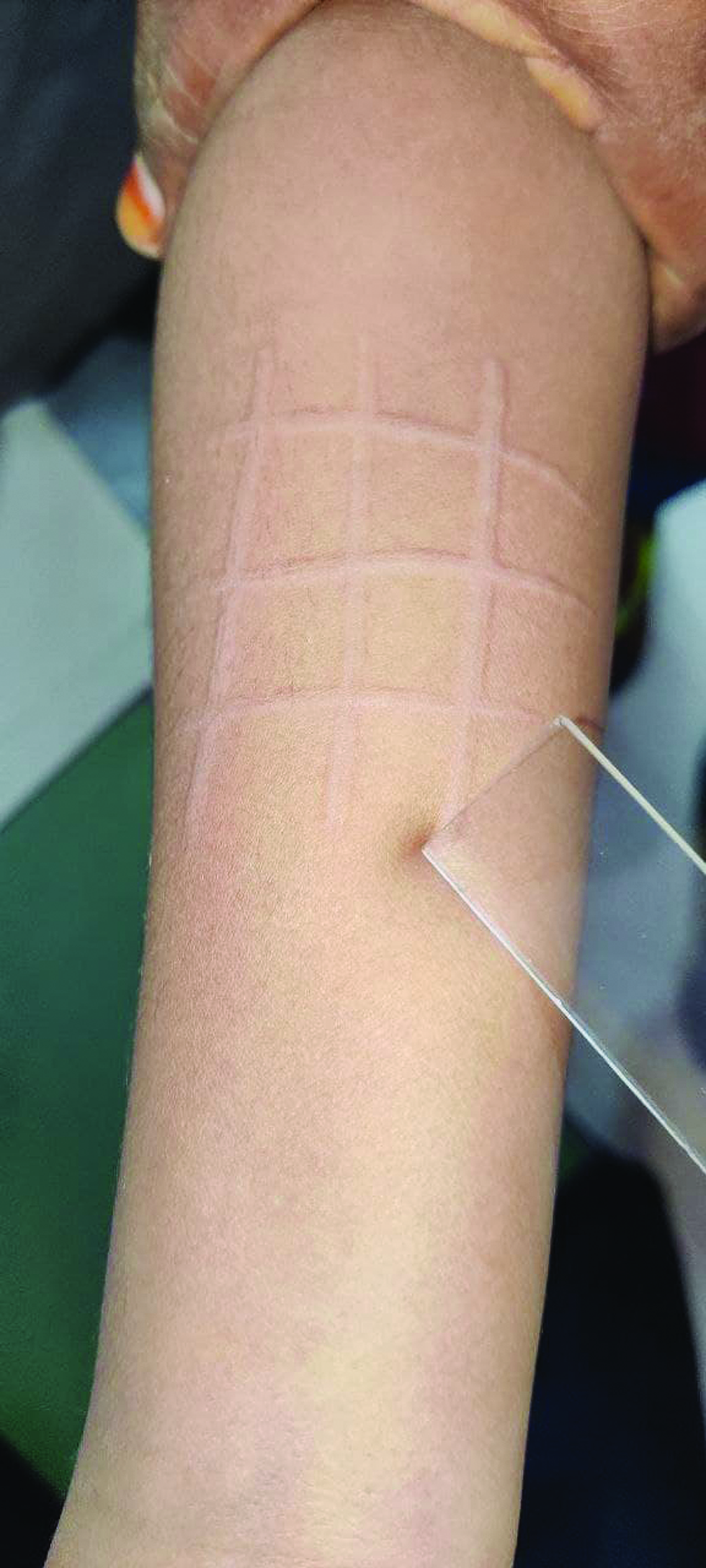
- Dermatographism elicited using a glass slide.
Role in diascopy:
Diascopy or vitropression is a common office procedure where the application of pressure with help of a diascope usually a transparent glass slide will lead to alteration of the skin lesion, mostly used for the following purposes.
In differentiating vascular from nonvascular lesions and observing for the blanching response in case of presence of vascularity in lesions such as telangiectasia, angioma, vascular tumors, and malformations.[9]
To differentiate purpura (due to extravasation of blood) due to vasculitis which does not blanch from reactive erythema due to other causes [Figure 3].
For differentiating urticaria from cases of urticarial vasculitis which does not blanch.[3]
In differentiating nevus anemicus from nevus depigmentosus and vitiligo. The former lesions blanch and the edges are lost whereas the latter remains the same.[10]
It can be used for the demonstration of apple jelly nodules which are yellowish-brown nodules seen on diascopy seen classically in lupus vulgaris but also in cases of lupoid leishmaniasis, lupoid rosacea, sarcoidosis, granuloma faciale, and pseudolymphoma.[11]
It can be used for making the hypopigmented macules of the lip prominent and also for differentiating macules of vitiligo which appears uniform white with convex margins from that of postinflammatory hypopigmentation which appears tan brown with uneven or jagged margins.[12]
It can be used for assessing the vascularity of lesions before a biopsy or surgical excision.
It can make the lesions look more prominent in lichen planus, lichen sclerosus et atrophicus, and seborrheic keratosis.[10]
In the case of xanthelesma like conditions, it can make the yellow color more prominent, such as xanthomas, necrobiosis lipoidica, and pseudoxanthoma elasticum.[9]

- Diascopy demonstrating non blanchable purpura.
Specimen collection for STI:
Glass slide is useful for most of the specimen collection in sexually transmitted infections [Figures 4 and 5 ]. In the case of syphilitic chancre, the glass slide can be directly pressed onto the moist lesions and serum along with the treponemes collected and covered with a coverslip and examined in direct light microscopy or darkfield microscopy. In the case of chancroid, a sterile swab is rolled onto the base of the ulcer and the swab is re-rolled onto the glass slide in the opposite directions. It can also be used for the preparation of crush specimens of tissue collected in the case of donovanosis (Rajam and Rangiah method).[13]
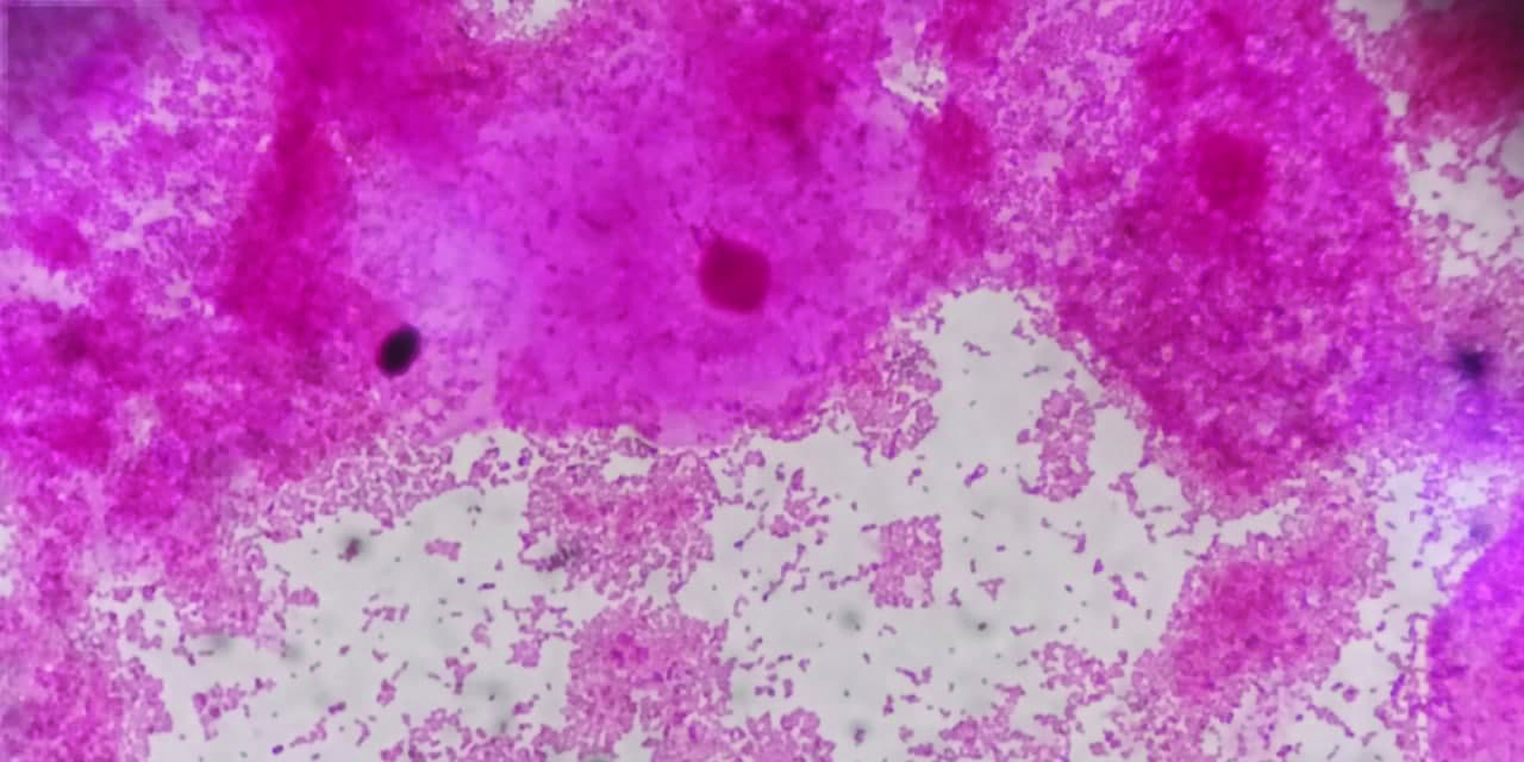
- Gram stain of discharge in bacterial vaginosis showing clue cells.
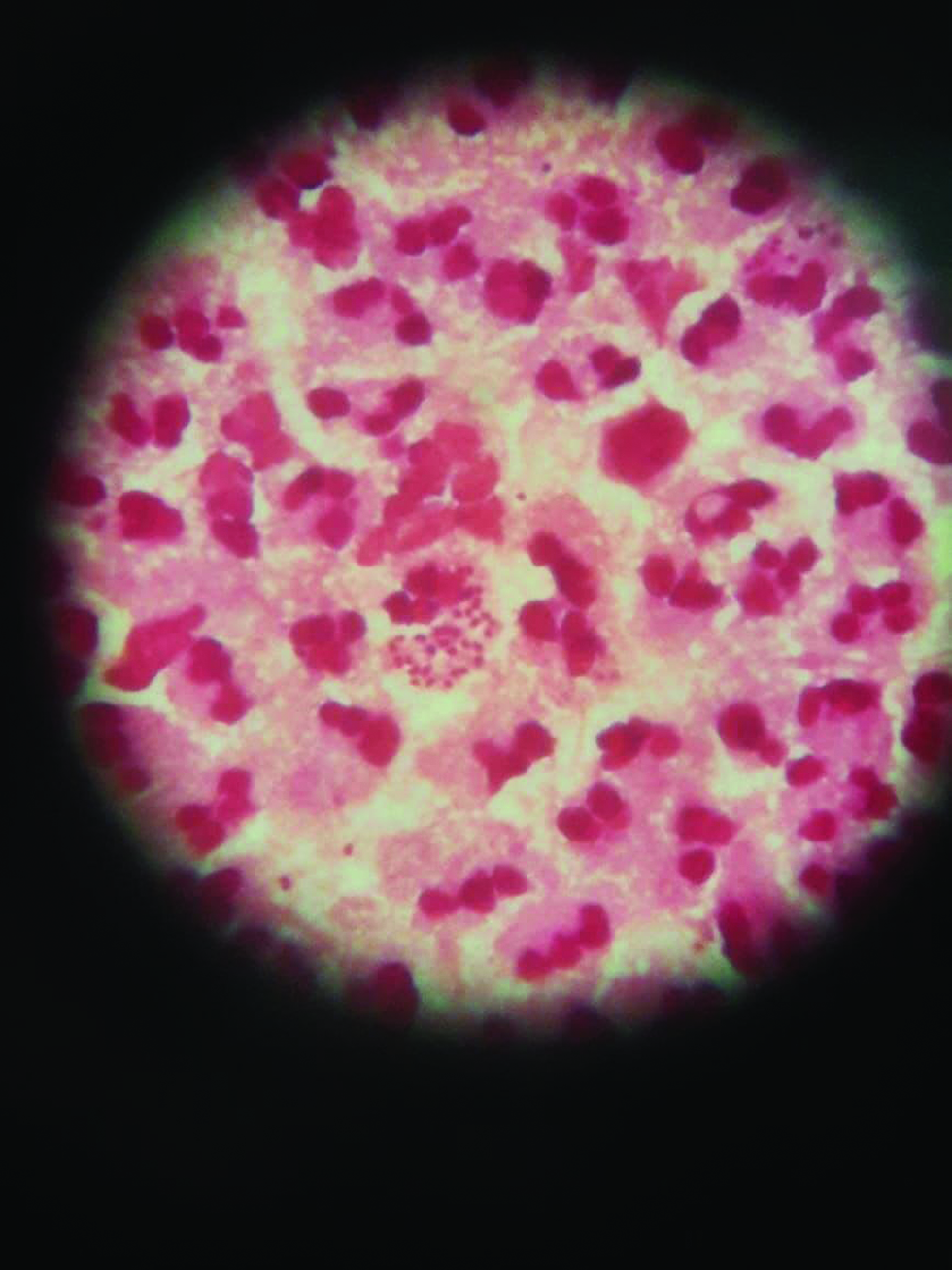
- Gram stain of urethral discharge showing gram-negative intracellular diplococci in gonorrhea.
Skin surface biopsy:
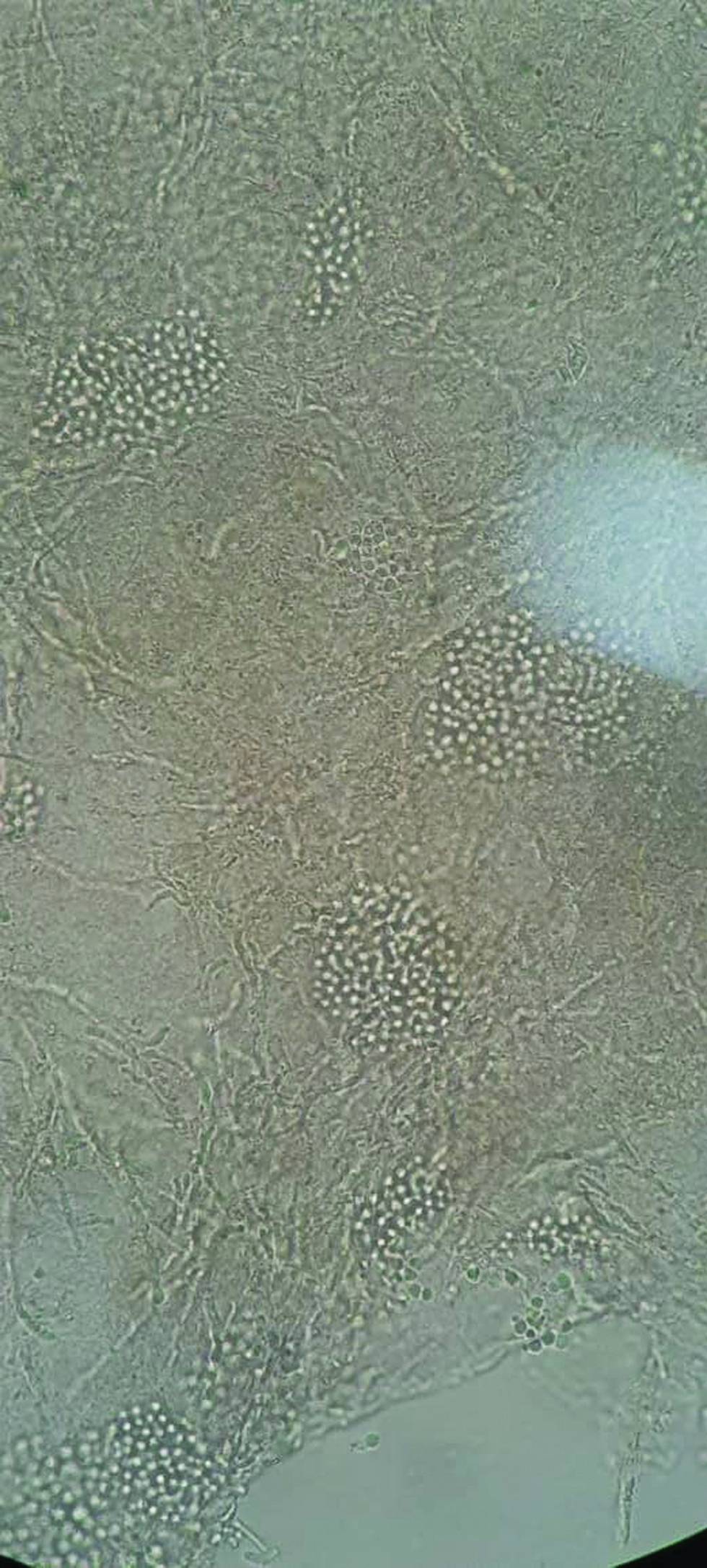
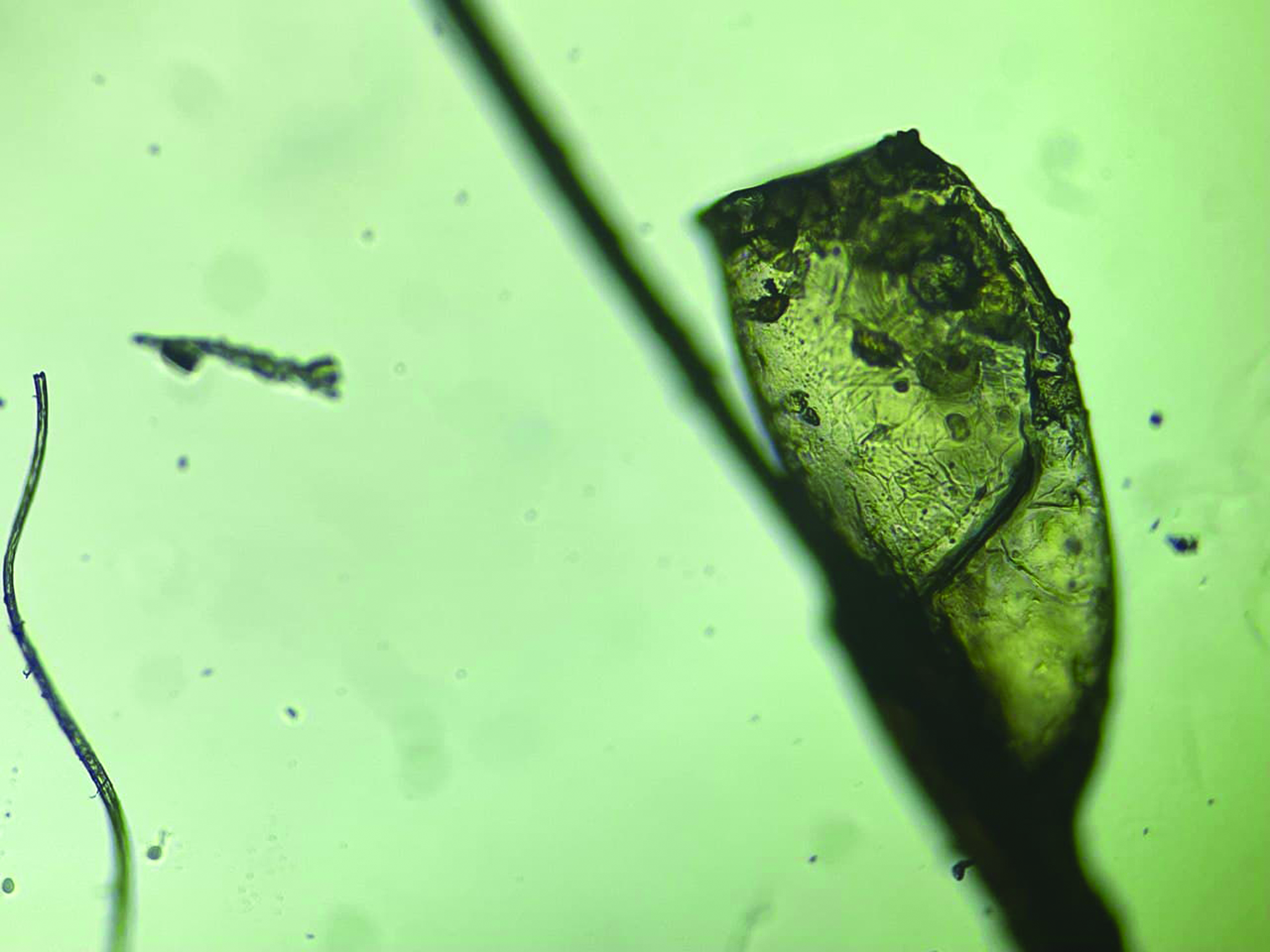
This technique was first introduced by Marks and Dawber in the year 1972, also referred to as superficial cyanoacrylate biopsy (SCAB), employs glass slide and cyanoacrylate glue (superglue) for the examination of superficial epidermal structures, especially stratum corneum. Here a drop of cyanoacrylate glue is placed onto the glass slide and pressed onto the skin lesions for about 30 seconds. It is then detached with force and observed immediately under a light microscope. Mostly used for the demonstration of superficial parasitosis such as scabies and demodicosis [Figures 6]. It might also be useful in the diagnosis of superficial fungal infection, inflammatory conditions such as seborrheic dermatosis, pityriasis rosea, and skin neoplasms such as seborrheic keratosis, dysplastic nevus, and melanoma.[14,15]

- Skin surface microscopy using cyanoacrylate glue showing the presence of Demodex folliculorum.
Role in assistive dermoscopy:
Dermoscopy is a useful tool in the diagnosis of common skin disorders and is often referred to as the stethoscope of the dermatologist. However, it is expensive and not everybody can afford, hence a novel modified technique has been employed for achieving similar magnification. It makes use of echo gel, which is placed onto the skin lesions, over which a glass slide is mounted and then it is illuminated with the light source at an oblique angle, and the lesions are viewed under an eyepiece lens. Also, glass slides can serve as a barrier between the dermoscope and skin lesions and hence prevent direct contact and contamination, especially in the case of infective lesions and genital examination.[16]
Side lab procedures:
It is also used frequently as part of common side lab procedures such as KOH examination for fungal infections, cytological examination using Tzanck smear, Ziehl-Neelsen staining for identification of acid-fast bacilli, and mineral oil mount for scabies infestation and pediculosis [Figures 7-14].[3]
- KOH mount showing “Ziti and meatballs appearance” of pityriasis versicolor.

- KOH mount showing broad aseptate branching hyphae in mucormycosis.

- Tzanck smear showing acantholytic cells in pemphigus vulgaris.

- Ziehl-Neelsen staining showing acid-fast bacilli suggestive of Mycobacterium Leprae.

- Mineral oil mount demonstrating mite and eggs of Sarcoptes scabiei var. hominis.

- Pthirus Pubis or crab louse observed under 10× magnification.

- Head louse or pediculosis capitis with blood meal observed under a microscope (10×).
- Nit of pediculosis capitis observed under high power (40×).
Hair examination:
Hair examination with KOH mount can be used for tinea capitis to differentiate endothrix and ectothrix infections. In the process of trichogram, the plucked hairs are arranged over the glass slide and then taped firmly to it. The various parts of the hair are then analyzed especially the root for anagen to telogen ratio and to look for dystrophic hairs, the shaft for uniformity, external aggression and substance deposits, and the tip for any breakage or distinguishing vellus from regrowing hairs [Figures 15-17].[17,18]
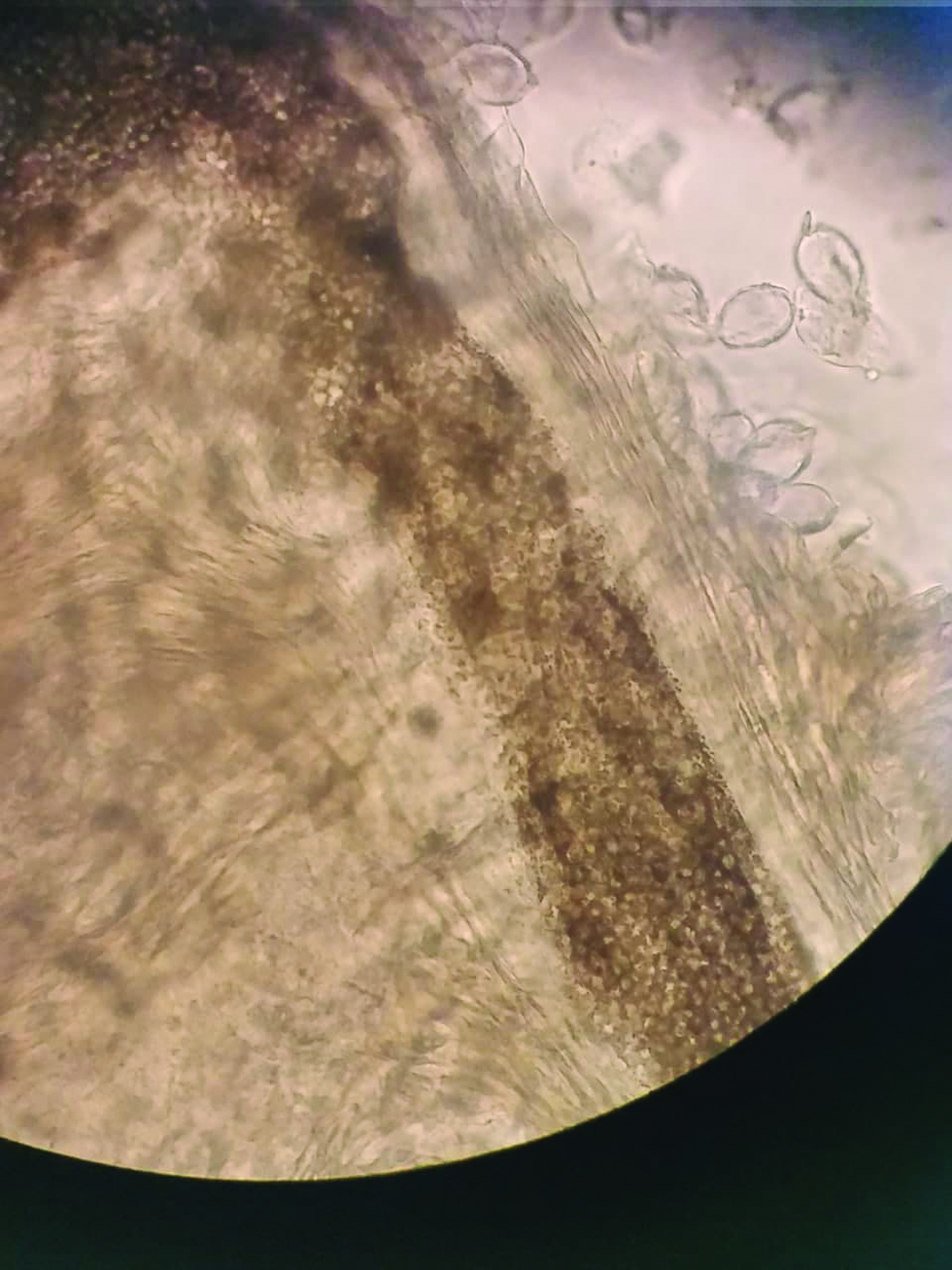
- Hair shaft KOH mount showing “sack of marbles” appearance of fungal spores in endothrix infection.

- Telogen hair bulb with club-like appearance without the root sheath.
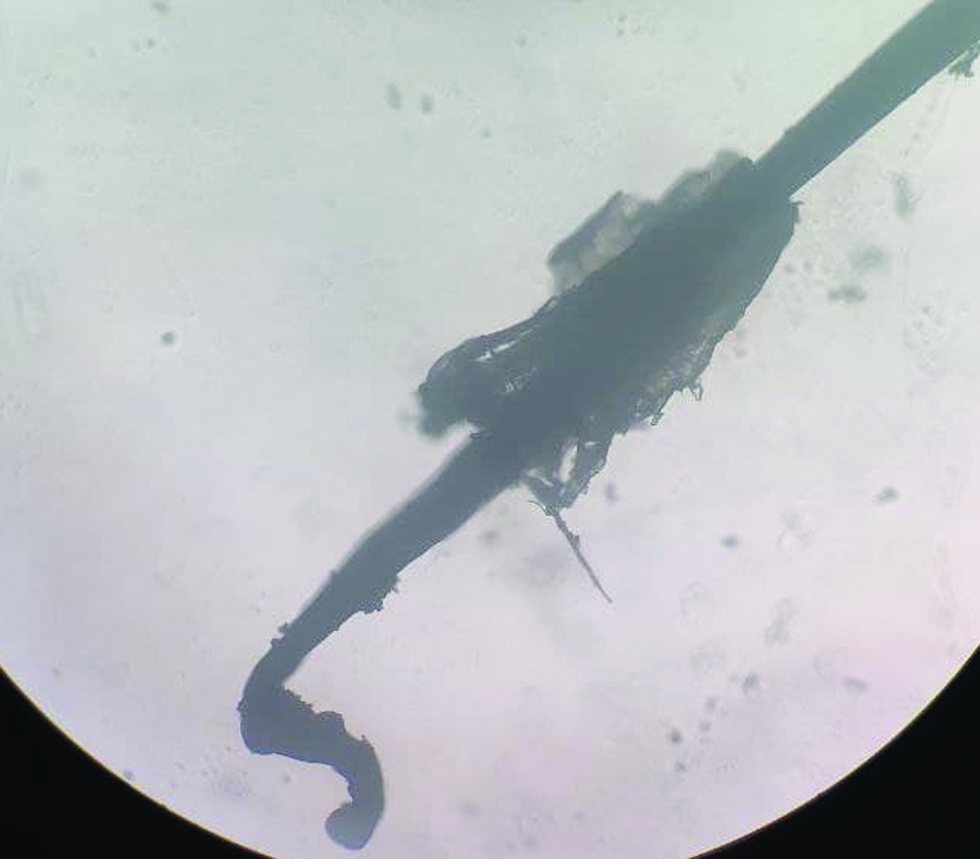
- Anagen hair with curved appearance and pigmented root sheath.
CONCLUSION
Thus, enumerating the various uses of the glass slide, it is a much-needed tool for the dermatologist in the day-to-day practice for the diagnosis of common skin disorders.
Declaration of patient consent
Patient’s consent is not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Was It Auspitz’s Sign? SKIN J Cutan Med [Internet] 2019. [cited 2021 Jul 10];3. Available from:
- [Google Scholar]
- Auspitz sign is not sensitive or specific for psoriasis. J Am Acad Dermatol. 1990;22:1079-81.
- [CrossRef] [PubMed] [Google Scholar]
- Textbook of Dermatology, Venereology and Leprology e-book. Elsevier Health Sciences 2015::617.
- [Google Scholar]
- Scaly signs in dermatology. Indian J Dermatol Venereol Leprol. 2006;72:161-4.
- [CrossRef] [PubMed] [Google Scholar]
- Phenomena in dermatology. Indian J Dermatol Venereol Leprol. 2011;77:264-75.
- [CrossRef] [PubMed] [Google Scholar]
- Investigative and clinical studies with diascopy in dermatology. AMA Arch Derm. 1957;75:699-705.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical value of diascopy and other non-invasive techniques on differential diagnosis algorithms of oral pigmentations: A systematic review. J Clin Exp Dent. 2016;8:e448-58.
- [CrossRef] [PubMed] [Google Scholar]
- Granuloma faciale: An unusual diascopic finding. Indian Dermatol Online J. 2016;7:174-6.
- [CrossRef] [PubMed] [Google Scholar]
- Diascopy in oral lesions: An old algorithm revisited. J Dent Oral Biol. 2017;2:1114.
- [Google Scholar]
- Methods of specimen collection for the diagnosis of STIs. Indian J Dermatol Venereol Leprol. 2007;73:129-32.
- [CrossRef] [PubMed] [Google Scholar]
- Cyanoacrylate skin surface stripping and the 3s-biokit advent in tropical dermatology: A look from liège. Sci World J. 2014;2014:462634.
- [CrossRef] [PubMed] [Google Scholar]
- Two consecutive standardized skin surface biopsies: an improved sampling method to evaluate demodex density as a diagnostic tool for rosacea and demodicosis. Acta Derm Venereol. 2017;97:242-8.
- [CrossRef] [PubMed] [Google Scholar]
- Self-assembly of a simple low-cost dermoscope for examination of skin lesions. Dermatol Pract Concept. 2013;3:35.
- [CrossRef] [PubMed] [Google Scholar]
- Hair evaluation methods: Merits and demerits. Int J Trichology. 2009;1:108-19.
- [CrossRef] [PubMed] [Google Scholar]
- Hair and scalp evaluation: The trichogram. Actas Dermosifiliogr. 2013;104:867-76.
- [CrossRef] [PubMed] [Google Scholar]





