Translate this page into:
Extramammary Paget’s disease in skin of color

*Corresponding author: K. J. Karrunya, Department of Dermatology, Sundaram Medical Foundation, Dr. Rangarajan Memorial Hospital, Chennai, Tamil Nadu, India. coolkarru@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sarveswari K, Karrunya K, Ponvannan P, Karthik V. Extramammary Paget’s disease in skin of color. CosmoDerma. 2024;4:56. doi: 10.25259/CSDM_35_2024
Dear Sir,
Although skin color plays a highly significant role in the manifestation of cutaneous disorders, traditional dermatological literature has largely focused on the presentation of skin conditions in white skin. This has led to lesser confidence in treating such disorders in black and brown demographics.[1] While recent literature has attempted to increase the diversity of images available for the more common dermatological conditions, there is still a considerable lack of knowledge about the presentation of rarer disorders in colored skin. We present one such case in this letter, involving a patient with clinical symptoms corresponding to Extramammary Paget’s Disease (EMPD) – a relatively rare pre-invasive skin cancer, with low rates of malignancy.[2]
A 58-year-old female patient presented with a one-year history of perianal patches. She had previously been treated with topical steroids and antifungals but with no improvement. Over the past month, she had noted an increase in the size of the lesion. The patient had no recorded diabetes mellitus or history of sexually transmitted infections. There was a family history of esophageal cancer. Prior investigations had included a colonoscopy for anal pain and a guided abdominal ultrasound, both of which were normal from gastro-intestinal and genitourinary perspectives. Routine laboratory investigations too were normal. A recently conducted positron emission tomography scan displayed mild metabolically active cutaneous thickening at the perianal region. Clinical examination of the patient showed an erythematous, hyperpigmented plaque, with well-demarcated but irregular edges. The lesions extended from the perianal region up to the vagina [Figures 1 and 2]. No other lesions were found elsewhere on the body. Based on the clinical findings, the initial diagnoses considered were erosive lichen planus, Crohn’s disease, and EMPD. Erosive lichen planus was prospectively ruled out due to the lack of effectiveness of the steroid treatment. Crohn’s disease too was ruled out by the consultant gastroenterologist due to the lack of gastrointestinal (GI) abnormalities. A biopsy was then performed to confirm the diagnosis, and a specimen was sent to histopathology. The sample showed basket weaving orthokeratosis and acanthosis. There was also an invasion of the epidermis by big cells with pale cytoplasm and pleomorphic nuclei, which extended down to the dermis as well ([Figure 3] – Hematoxylin and Eosin section, ×10). A special stain for mucin was positive. Immunohistochemistry was not done. This pattern of histopathology, along with the spread of the lesion, led to a conclusive diagnosis of EMPD.[2] The patient was then referred to the oncologist for further management. An important point to note here is the pigmented nature of the lesion in this patient.

- Erythematous, hyperpigmented plaque with well-demarcated but irregular edges in the perianal region.

- Erythematous, hyperpigmented plaque with well-demarcated but irregular edges in the perianal region.
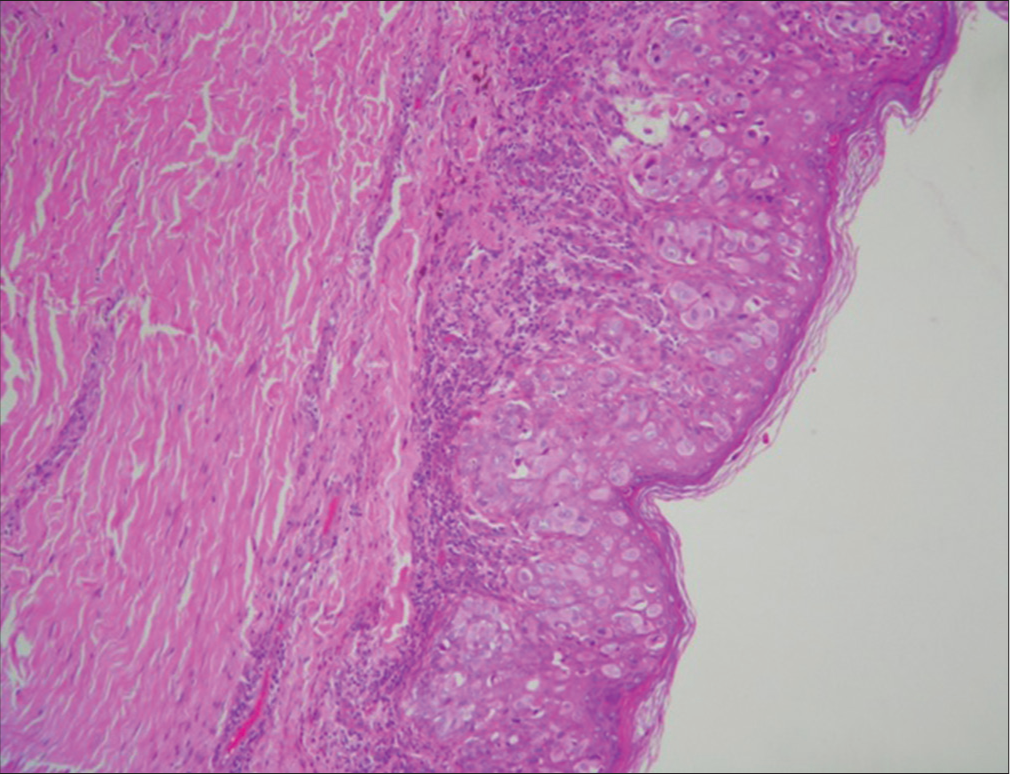
- Hematoxylin and eosin, ×40 invasion of the epidermis by pagetoid cells.
According to traditional literature, EMPD is characterized by erythematous, well-demarcated, and itchy plaques appearing in areas with a high abundance of apocrine sweat glands. The lesions occur most frequently on the vulva, but can also appear in the peri-anal, scrotal, perineal, and penile skin. The pigmented type of EMPD is uncommon and can result from increased dendritic melanocytes, intra-cytoplasmic melanin in the pagetoid cells or the presence of melanophages.[3] The three patterns of EMPD noted in the literature include the in situ epithelial form without any associated carcinoma, the epithelial form associated with adnexal carcinoma, and the one associated with GI tract malignancy or genitourinary malignancy.[4] However, presentations of pigmented lesions, combined with a family history of malignancy, have been reported in a few cases of colored skin. The condition was often misdiagnosed in such instances,[5,6] and only through biopsy and histopathology was EMPD considered as a definitive diagnosis. In our presenting case too, there had been previous instances of misdiagnosis and ineffective treatment at other health centers before the final diagnosis was made. This, in our opinion, directly reflects on the lack of literature detailing atypical presentations and rarer disorders in skin of color. Given the risk of underlying malignancy associated with EMPD, the consequence of mismanagement remains high.
It is therefore our opinion that the condition should be considered with a high degree of suspicion in menopausal women or patients with a history of cancer, presenting with similarly irregular, pigmented, and well-demarcated rashes. It is also important to consider updating dermatological images to be more inclusive of the skin of color, especially for such pigmented disorders, to prevent late diagnosis and risk further systemic involvement.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Visual racism in internet searches and dermatology textbooks. J Am Acad Dermatol. 2021;85:1348-9.
- [CrossRef] [PubMed] [Google Scholar]
- Extramammary Paget disease In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2024.
- [Google Scholar]
- Extramammary Paget's disease. Indian J Dermatol Venereol Leprol. 2005;71:417-20.
- [CrossRef] [PubMed] [Google Scholar]
- Pigmented extramammary Paget's disease of the axilla mimicking melanoma: Case report and review of the literature. J Cutan Pathol. 2009;36:995-1000.
- [CrossRef] [PubMed] [Google Scholar]
- Pigmented extramammary Paget disease of the thigh mimicking a melanocytic tumor: Report of a case and review of the literature. J Cutan Pathol. 2014;41:529-35.
- [CrossRef] [PubMed] [Google Scholar]





