Translate this page into:
Eccrine spiradenoma localized to the area of striae distensae – “locus minoris resistentiae”

*Corresponding author: Pradeep S. Nair, Department of Dermatology and Venereology, Government T D Medical College, Alappuzha, Kerala, India. dvmchtvm@yahoo.co.in
-
Received: ,
Accepted: ,
How to cite this article: Nair PS, Dhanesh D, Devi PL. Eccrine spiradenoma localized to the area of striae distensae – “locus minoris resistentiae”. CosmoDerma. 2025;5:37. doi: 10.25259/CSDM_23_2025
Dear Sir,
A 17-year-old male presented with a lesion on the upper left chest for a three-month duration. The lesion first started as a skin-colored papule with slight tenderness on the upper left chest. There was no preceding trauma. There was no history suggestive of oozing, crusting, or bleeding. Recently, the patient had lost weight due to dieting and exercise and consequently developed multiple linear whitish streaks, bilaterally on the upper lateral chest extending to the axilla before the onset of the skin lesion. There was no family history of similar lesions. There was no history of any systemic illness.
On examination, there were multiple discrete linear whitish atrophic plaques with wrinkling extending from the lateral pectoral region to the anterior axillary fold, bilaterally suggestive of striae distensae [Figure 1]. The middle of the lower striae distensae on the left pectoral region had an ill-defined skin-colored to slight bluish-colored papule with irregular margins and tender to palpation [Figure 1]. There were no lesions elsewhere. Systems were within normal limits. Dermoscopy was non-contributory. Serological examinations were normal. An excision skin biopsy demonstrated on scanner view, an atrophic epidermis, and the dermis packed with well-defined basophilic tumor lobules surrounded by a capsule and intervening stroma with scant infiltrate [Figure 2]. The high power demonstrated the tumor lobules packed with cords of cells with two types of cells: Round cells with strongly staining basophilic nuclei and round cells with pale staining nuclei, along with ductal structures suggestive of eccrine spiradenoma (ES) [Figure 3]. Before the onset of ES, the patient had striae distensae. In between the lesions of striae distensae, there were normal areas of skin [Figure 1]. The localization of ES on the striae distensae rather than the intervening normal skin is not a coincidence. Therefore, we made a final diagnosis of ES arising from stria distensae due to “locus minoris resistentiae” (LMR).

- Skin-colored papule with bluish tinge on striae distensae.
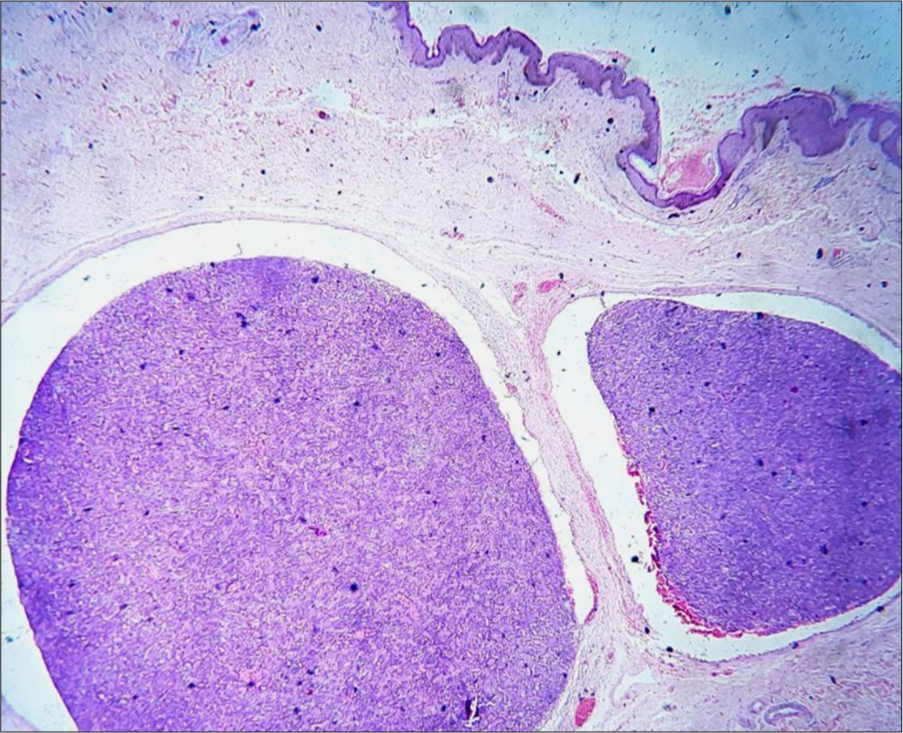
- Multiple basophilic tumor lobules surrounded by capsule, hematoxylin and eosin ×40.
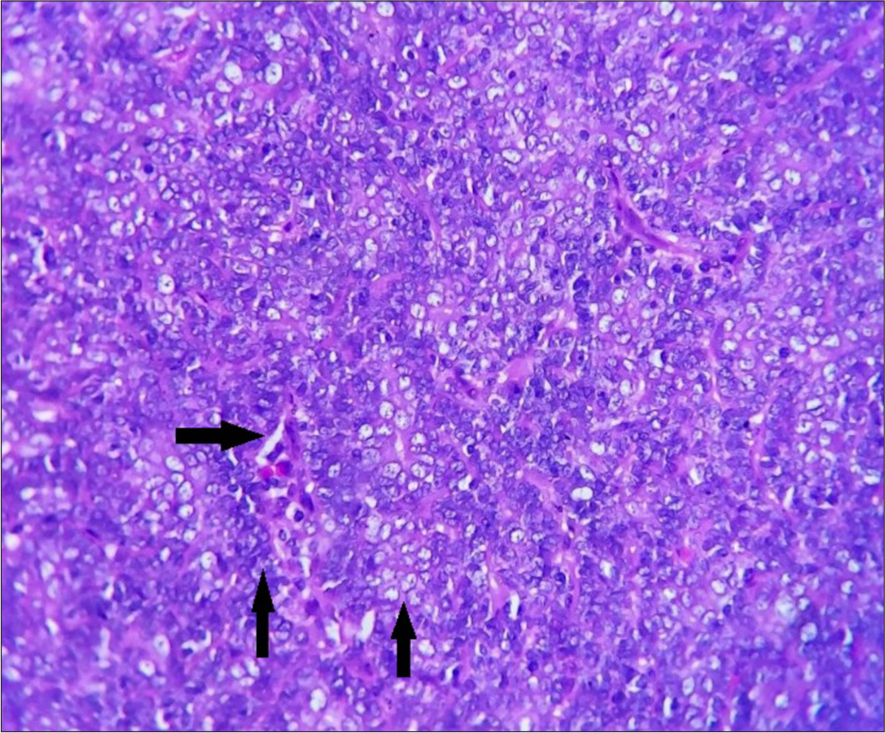
- High power showing cells with basophilic nuclei (left vertical arrow) and cells with pale staining nuclei (right vertical arrow) and ductal structures (horizontal arrow), hematoxylin and eosin ×400.
ES is a benign tumor of the eccrine glands arising from the eccrine gland ducts, one of the painful tumors of the skin and usually localized to the proximal extremities and trunk. They are usually solitary and present with skin colored to bluish papules and nodules with a characteristic histopathology and malignant transformation is <0.3%. An ES arising from an area of striae distensae qualifies for the concept of LMR. LMR means “sites of less resistance.”[1] These sites of less resistance can be the future nidus for other unrelated dermatoses to be localized here. These sites can be areas of striae distensae, scar tissue, healed areas of previous dermatosis, or sites of previous injury. The isomorphic response of Koebner and Wolf ’s isotopic response is also attributed to the concept of LMR.[2] The isomorphic response of Koebner refers to the phenomenon of isomorphic lesions occurring in areas of trauma as in the cases of lichen planus and psoriasis, while Wolf ’s isotopic response refers to a dermatosis occurring in the area of previous scar tissue of an unrelated dermatosis, the classical example being sarcoidosis occurring in herpes zoster healed scars. The exact mechanism of LMR is not elucidated. Various mechanisms have been postulated. Damage to the dermal matrix in scar tissues makes these areas less resistant and encourages the trafficking of T-cells, especially T-memory cells to these areas, hence the appearance of these dermatoses.[3] Damage to the microcirculation following inflammation and subsequent recall has also been proposed. The latest is the neural hypothesis, which states that an initial injury releases neuropeptides and these same neuropeptides are released again by new dermatoses due to abnormal immune trafficking of cells.[4] Numerous dermatoses such as granulomatous, benign and malignant tumors, infectious dermatoses, and inflammatory dermatoses have been reported to occur in scar tissue and striae distensae.[2] We are reporting an interesting case of ES arising in an area of striae distensae, the first of its kind to the best of our knowledge.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Locus minoris resistentiae: An old but still valid way of thinking in medicine. Clin Dermatol. 2014;32:553-6.
- [CrossRef] [PubMed] [Google Scholar]
- Extensive verrucae over healed pemphigus vulgaris lesions in an immunocompetent female: A rare presentation of wolf 's isotopic response. Indian J Dermatol. 2020;65:211-3.
- [CrossRef] [PubMed] [Google Scholar]
- Yoga sign-A locus minoris resistentiae to remember. Indian Dermatol Online J. 2021;12:760-1.
- [CrossRef] [PubMed] [Google Scholar]
- Wolf 's isotopic response: Report of a case and review of literature. Indian J Dermatol. 2014;59:275-82.
- [CrossRef] [PubMed] [Google Scholar]





