Translate this page into:
Dermoscopy-histopathology correlation of cutaneous small-vessel vasculitis

*Corresponding author: Vishal Gaurav, Department of Skin and VD, Maulana Azad Medical College, New Delhi, India. mevishalgaurav@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Gaurav V, Gowda P, Bahadur A, Tyagi H, Dev T, Barman KD. Dermoscopy-histopathology correlation of cutaneous small-vessel vasculitis. CosmoDerma. 2024;4:90. doi: 10.25259/CSDM_113_2024
Dear Sir,
Cutaneous small-vessel vasculitis (CSVV) presents a diagnostic challenge due to its diverse clinical manifestations and the overlap with other purpuric dermatoses. We report the details of clinical presentation, dermoscopic findings, and histopathological correlation in a young boy with CSVV. Dermoscopy is increasingly recognized as a valuable tool in the assessment of inflammatory skin conditions, providing non-invasive insights that complement histopathological examination.
A 9-year-old boy presented with a three-day history of purpuric lesions primarily located on the lower extremities. The patient reported a preceding upper respiratory tract infection, but denied any history of drug intake, insect bites, or recent vaccinations. The child did not have any systemic symptoms such as fever, abdominal pain, bleeding episodes, or joint swelling. On physical examination, the patient exhibited numerous non-blanchable discrete purpuric macules and papules which were coalescing to form larger macules and plaques. These lesions were predominantly located on the extensor surfaces of the legs [Figure 1]. There was no evidence of mucosal involvement, and other systemic examinations were unremarkable. Polarized dermoscopy (Heine DELTAone) of the purpuric lesions revealed a pattern of red to purple dots and globules on a reddish background [Figure 2]. Laboratory investigations, including complete blood count, liver and renal function tests, and urinalysis, were within normal limits, excluding any hematological or renal complications. A skin biopsy was performed on the most recent lesion to confirm the diagnosis. Histopathology revealed fibrinoid necrosis of vessel walls, neutrophilic infiltration, leukocytoclasia, and perivascular infiltrate composed of neutrophils, lymphocytes, and histiocytes involving the vessels in the superficial and mid dermis. Extravasation of red blood cells (RBCs) and dermal edema was also noted [Figures 3 and 4]. Based on clinical, dermoscopic, and histological findings, the boy was diagnosed as a case of CSVV. The parents were counseled about the disease’s nature and prognosis, and the child was started on ibuprofen (200 mg three times/day) and topical mometasone furoate 0.1% cream, which resulted in the resolution of the lesions within 1 week.
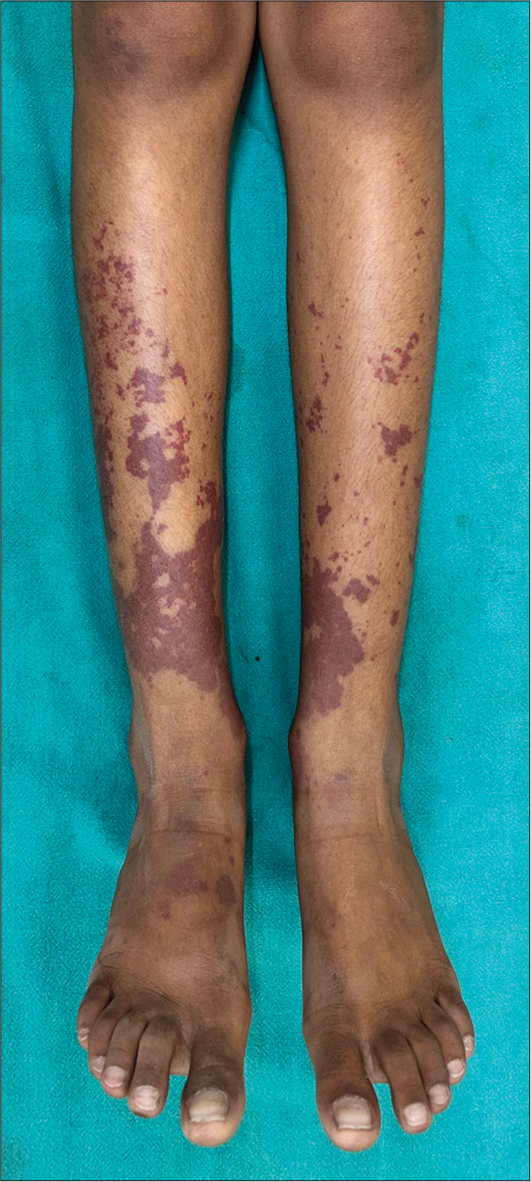
- Multiple non-blanchable discrete purpuric macules and papules coalescing to form larger macules and plaques on the extensor surfaces of the legs.
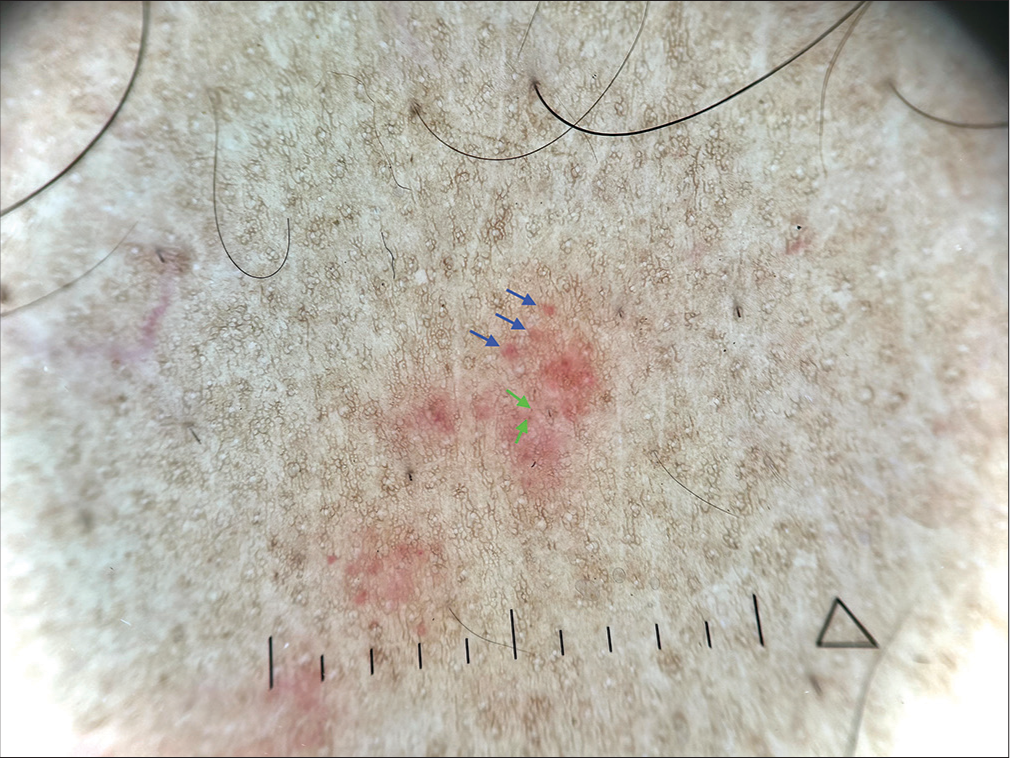
- Polarized dermoscopy (Heine DELTAone) of the purpuric lesions showing a pattern of red dots (green arrows) and globules (navy blue arrows) on a reddish background (×20).
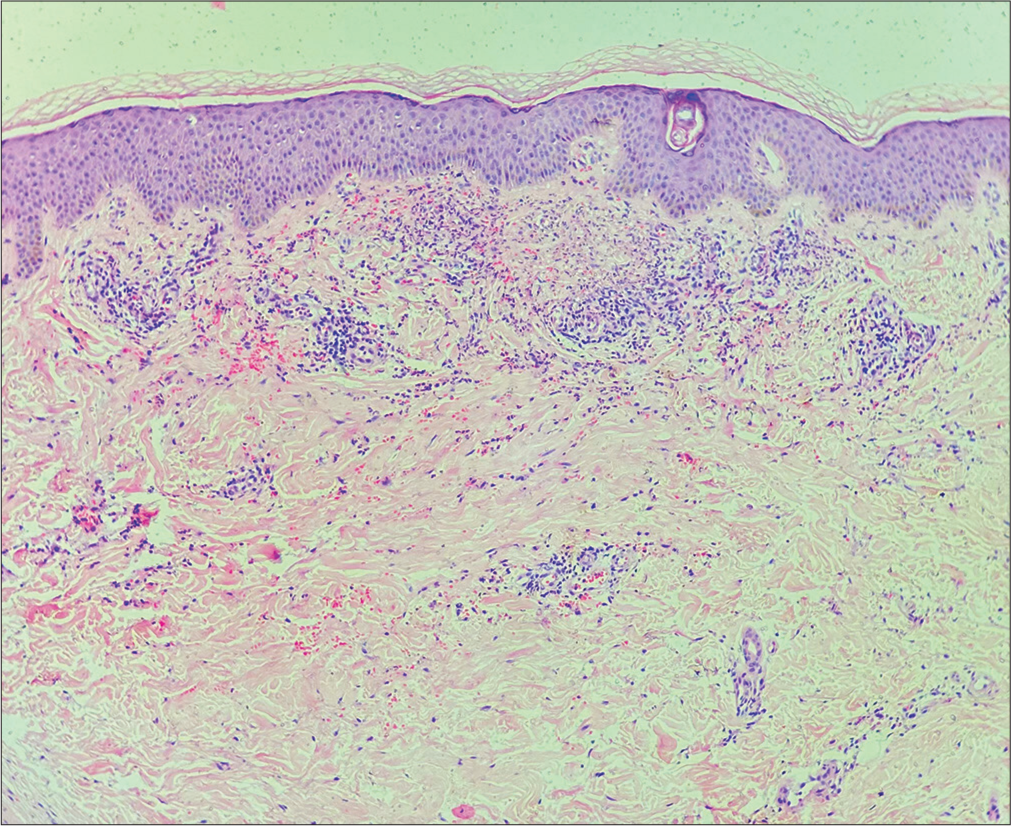
- Histological section showing fibrinoid necrosis of vessel walls, neutrophilic infiltration, leukocytoclasia, and perivascular infiltrate involving the vessels in the superficial and mid dermis. Extravasation of red blood cells and dermal edema is also prominent (Hematoxylin and eosin; ×100).
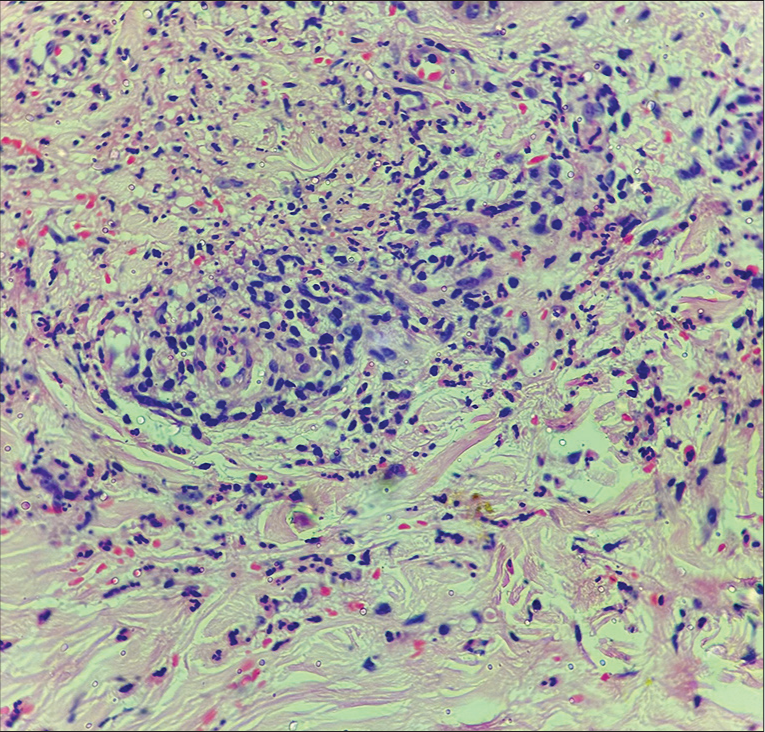
- Histological section showing fibrinoid necrosis and neutrophilic infiltration of vessel wall with leukocytoclasia. The perivascular infiltrate is composed of neutrophils, lymphocytes, and histiocytes (Hematoxylin and eosin; ×400).
Vazquez-Lopez et al. have described four fundamental dermoscopic patterns for purpuric lesions: Homogeneous, mottled, perifollicular, and epidermal purpuric. The homogeneous pattern is indicative of non-inflammatory purpura, such as bleeding diathesis, and is characterized by extensive, uniform, and structureless purpuric regions. In contrast, the mottled pattern, which features numerous small, speckled, indistinct purpuric blotches or globules on a purple to orange-brown background, is associated with inflammatory conditions such as leukocytoclastic vasculitis and pigmented purpuric dermatoses (PPD). A perifollicular pattern is characteristic of scurvy, while an epidermal pattern is typically observed in subcorneal/subungual hemorrhages and eczema.[1-3]
In the early stages of cutaneous vasculitis, lesions usually present with a dull red background along with red globules and dots. As the condition progresses to more established lesions, a red to red-purple background becomes apparent, along with white and yellow structureless areas, red globules, and red dots.[4] The red background seen in dermoscopy is mainly due to the presence of dilated blood vessels, though dermal edema and collagen may also contribute to this appearance. White and yellow structureless areas are indicative of a “mass effect” caused by cellular aggregates in the dermis, where dense, compact aggregates produce a yellowish to yellow-orange color, and sparser aggregates appear yellow-white to white. Red dots and globules are histologically linked to RBC extravasation, with the terms “dots” and “globules” differentiating these structures primarily by size.[2-4] A cross-sectional study explored the dermoscopic features of CSVV and their correlation with histopathological findings. Involving 30 patients confirmed by histopathology and direct immunofluorescence, the study recorded dermoscopic features of both early/evolving and established lesions. Early/evolving lesions consistently showed a dull red background, with red globules and red dots observed in fewer cases. Established lesions displayed a red background, white and yellow structureless areas, and red globules and dots. A significant association was found between red globules and RBC extravasation, and between white/yellow areas and perivascular infiltrates. Dermoscopy can be used to select an early lesion for biopsy and direct immunofluorescence.[4] Bakay et al. investigated the use of dermoscopy and machine learning (ML) to improve the diagnosis of cutaneous vasculitis. The study involved 89 patients with suspected CV, with dermoscopic images evaluated independently before biopsy. Three dermoscopic patterns (homogeneous, mottled, and meshy) and specific background colors (milky red and livedoid) were identified as significant markers for CV. ML models, including Decision Tree, Random Forest, and K-Nearest Neighbors, highlighted the background color and absence of scales as key diagnostic features.[5]
The PPD is the most common dermoscopic differential diagnosis of CSVV. The dermoscopic differences are summarized in Table 1.[6,7] The comparison underscores the distinct dermoscopic features of CSVV and PPD, highlighting the utility of dermoscopy in differentiating these conditions. The CSVV’s dermoscopic profile, marked by a red to red-purple background, lack of chronic pigmentary elements, and presence of yellow structureless areas, aligns with its acute inflammatory nature. In contrast, PPD’s features such as a yellow-brown background, specific vascular patterns, and pigmentary elements indicate chronicity and hemosiderin deposition.[4] Recognizing these differences is crucial for accurate diagnosis and appropriate management.
| Feature | CSVV | PPDs |
|---|---|---|
| Background color | Red dots and globules are present on a dull red (early/evolving lesions) and red to red-purple background (established lesions), due to vascular dilation and RBC extravasation without hemosiderin deposits | Red dots and globules are present on a yellow-brown or coppery-brown background, due to lymphohistiocytic infiltrate and hemosiderin deposits along with RBC extravasation |
| Vascular Patterns | No specific vascular patterns reported | Twisted red loops, red circles, linear serpentine, and annular-comma patterns present |
| Yellow Structureless Areas | Present, corresponding to dense neutrophilic infiltrates | Not typically described |
| Pigmentary Elements | Absent (no brown patches or reticular lines) | Brown patches and reticular lines present, due to hemosiderin deposition |
RBC: Red blood cell, CSVV: Cutaneous small-vessel vasculitis, PPD: Pigmented purpuric dermatoses
In conclusion, dermoscopy provides a crucial adjunct to clinical and histopathological evaluation in diagnosing CSVV. Recognizing specific dermoscopic patterns facilitates early diagnosis, monitoring of disease progression, and distinguishing from other conditions, thereby guiding appropriate therapeutic interventions. The integration of dermoscopy into routine clinical practice, alongside histopathological evaluation, enhances the diagnostic precision for inflammatory purpuric dermatoses.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Dermoscopic patterns of purpuric lesions. Arch Dermatol. 2010;146:938.
- [CrossRef] [PubMed] [Google Scholar]
- Importance of dermoscopy in differentiating common urticaria and urticarial vasculitis: A randomized control study. Clin Dermatol Rev. 2021;5:144-8.
- [CrossRef] [Google Scholar]
- Development of a clinical-dermoscopic model for the diagnosis of urticarial vasculitis. Sci Rep. 2020;10:6092.
- [CrossRef] [PubMed] [Google Scholar]
- Utility of dermoscopy in cutaneous small vessel vasculitis: Preliminary observations from a study of 30 cases. Indian Dermatol Online J. 2023;14:506-9.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopic features of cutaneous vasculitis. Dermatol Pract Concept. 2024;14:e2024051.
- [CrossRef] [PubMed] [Google Scholar]
- Progressive pigmented purpuric dermatosis in skin of color: A dermoscopic and histopathological correlation. Int J Res Dermatol. 2022;8:482-7.
- [CrossRef] [Google Scholar]
- Dermoscopic findings and the clinicopathologic correlation of pigmented purpuric dermatosis: A retrospective review of 60 cases. Ann Dermatol. 2021;33:214-21.
- [CrossRef] [PubMed] [Google Scholar]






