Translate this page into:
Cutaneous mosaicism: Segmental nevus depigmentosus with tuberous sclerosis

*Corresponding author: Dr. Muthu Sendhil Kumaran, Department of Dermatology, Venerology, and Leprology, Postgraduate Institute of Medical Education and Research, Chandigarh, India. drsen2017@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Singh S, Bhukamp A, Malhi K, Kumaran M. Cutaneous mosaicism: Segmental nevus depigmentosus with tuberous sclerosis. CosmoDerma. 2024;4:137. doi: 10.25259/CSDM_163_2024
Dear Sir,
Tuberous sclerosis is a rare genetic disorder presenting with a myriad of cutaneous and extracutaneous features, including pigmentary alterations. We describe an association between nevus depigmentosus (ND) and tuberous sclerosis complex (TSC) in a young man, which sheds light on shared pathomechanisms in both of these mosaic disorders.
A 20-year-old male presented with multiple asymptomatic skin-colored to reddish-brown papules over the nasolabial folds since childhood. A single, large hypopigmented patch over the trunk extending from the left waist to the buttocks and left thigh suggestive of segmental ND was observed. Additional findings included an irregular plaque suggestive of a shagreen patch and multiple ovoid hypopigmented non-scaly macules over the upper trunk and left forearm consistent with Ash-leaf macules [Figure 1a and b]. The latter were of varying size with feathery margins and lacked overlying leukotrichia. On diascopy, the lesions were non-blanchable. Dermoscopy of the larger hypopigmented patch revealed a subtle broken pigment network while smaller lesions revealed a diffuse whitish irregular area [Figure 2a and b]. He also had generalized tonic-clonic seizures in early childhood, but his developmental milestones were normal for his age. However, there was no history of similar complaints among family members. A skin biopsy was advised, but the patient refused it. Magnetic resonance imaging (MRI) of the brain revealed subependymal nodules in bilateral cerebral hemispheres [Figure 3]. Other investigations such as MRI abdomen were within normal limits. Based on the updated diagnostic criteria for TSC (2012) and Coup’s criteria, a diagnosis of tuberous sclerosis with segmental ND was made.[1,2] Genetic testing could not be done due to cost constraints. Table 1 summarizes key findings in index case.

- (a) A single, large hypopigmented patch with feathery margins over the trunk extending from left waist to buttock and thigh suggestive of segmental nevus depigmentosus, with an irregular thickened lesion suggestive of shagreen patch (box). (b) Multiple small reddish brown papules over the centrofacial region suggestive of angiofibromas (circle).
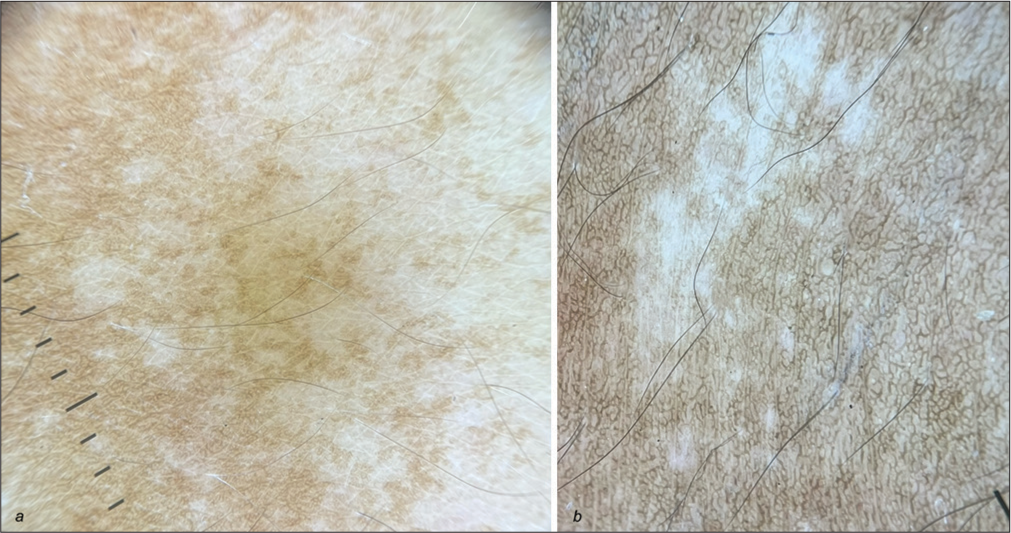
- (a) Dermoscopy of the larger hypopigmented patch revealed a subtle broken pigment network with feathery margins suggestive of nevus depigmentosus. DermLite 4, Polarized mode, Magnification ×10. (b) Dermoscopy of smaller hypopigmented lesions showing diffuse whitish irregular area without scales suggestive of ash-leaf macules. DermLite 4, Polarized mode, Magnification ×10.
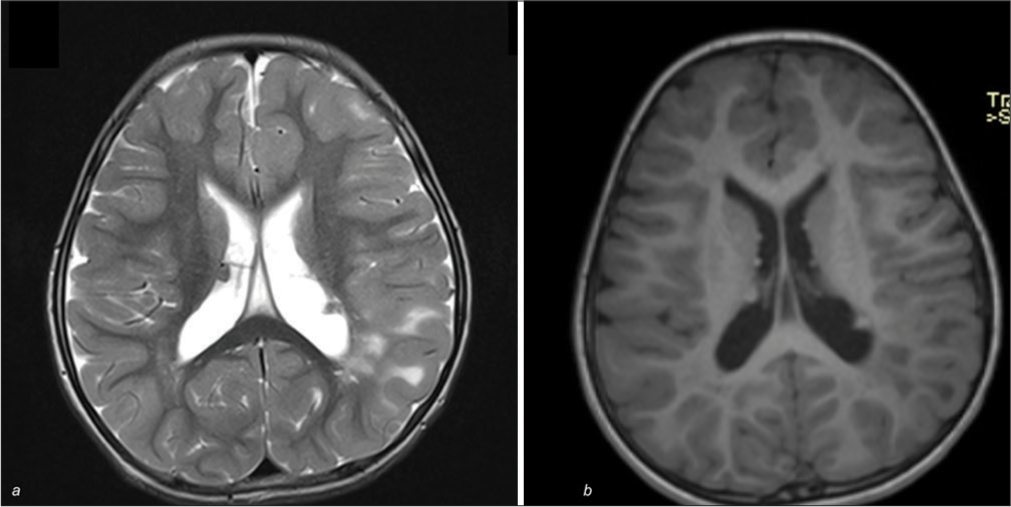
- (a and b) Magnetic resonance imaging of the brain showing subependymal nodules in the periventricular area on T2 and T1-weighted images.
| Clinical findings | Facial angiofibromas, ash-leaf macules, shagreen patch, segmental nevus depigmentosus, history of tonic-clonic seizures in childhood |
| Dermoscopy | Dermoscopy of the larger hypopigmented patch revealed a subtle broken pigment network while smaller lesions revealed a diffuse whitish irregular area |
| Imaging | MRI brain revealed subependymal nodules in bilateral cerebral hemispheres. MRI abdomen was within normal limits |
MRI: Magnetic resonance imaging
TSC is a multisystem autosomal dominant disorder affecting 1 in 10,000 newborns, with a median diagnosis around 15 months of age.[1] Cutaneous lesions serve as the earliest disease markers, including ash-leaf spots, facial angiofibromas, Shagreen patch, and periungual fibromas. Among these, ash-leaf spots appear first, at birth or during infancy, and are present in 90% of patients with TSC. These lesions present as ovoid hypopigmented, off-white macules measuring 1–5 cm, predominantly located over the trunk and buttocks. Other morphological patterns include confetti-like, thumbprint-shaped, or segmental lesions. Pigmentary abnormalities in TSC include multiple confetti such as skin lesions and hypopigmented macules occurring commonly over the extremities and trunk. ND is a congenital, non-progressive hypopigmented macule or patch with well-defined, serrated borders not traversing the midline. Clinically, three types have been described: Localized, segmental, and systematized form with localized being the most common. Diagnosis can be made using criteria established by Coup in 1976.[2] The criteria include leukoderma present at birth or appearing early in life, no change in the distribution of leukoderma throughout life, no alteration in texture or sensation in the affected area, and the absence of a hyperpigmented border.[2] Complete pigment loss with irregular, ill-defined margins and no perifollicular pigmentation suggest ash-leaf macules whereas perifollicular pigmentation, a subtle reticular pigment network, and diffuse whitish areas with serrated borders (pseudopods) suggest ND [Table 2].[3] In the index case, dermoscopy helped in the differentiation of ash-leaf macule and ND. In Ash leaf macules, histopathology shows fewer and smaller melanosomes, often aggregating in keratinocytes. In ND, melanosomes are normal in size, shape, and melanin content but fewer in number, aggregating within melanocyte vacuoles.[2] The association of ND in TSC has not been described in the literature and may suggest shared pathogenetic mechanisms. Both conditions have clinical and histological overlap and may show common extracutaneous features such as seizures, mental retardation, and skeletal defects. Recently, many genes implicated in phakomatous diseases such as NF1, TSC1, or TSC2 have been linked in a common biochemical pathway related to the mammalian target of rapamycin (mTOR) signaling.[4] Mutations causing loss of function in the TSC1 and TSC2 genes lead to mTOR complex 1 (mTORC1) hyperactivation and the onset of TSC. A common mechanism linking mTORC1 hyperactivation to neurological disorders has sparked interest due to the potential of mTOR inhibitors as therapies. A study suggested that in patients with TSC, constitutive hyperactivation of the mTOR pathway is associated with reduced skin pigmentation due to endoplasmic reticulum and mitochondrial oxidative stress, as well as lower melanization of melanosomes.[5] Interestingly, these features were also observed using electron microscopy in the case of ND along the lines of Blaschko.[6] The simultaneous occurrence of both entities explores further the possibility of the mTOR pathway in these entities. mTORC1 signaling pathways play a pivotal role in regulating cell growth through both sensing the energetic status of the cell and coordinating most metabolic processes that underlie growth. Understanding this association may provide new insights into the molecular underpinnings of these disorders and suggests the need for further research into the role of mTOR signaling in their pathogenesis including the treatment with targeted therapies such as sirolimus.
| Hypopigmented conditions | Dermoscopic features |
|---|---|
| Ash leaf macules | Complete pigment loss with irregular, ill-defined feathery margins and no perifollicular pigmentation |
| Nevus depigmentosus | Perifollicular pigmentation, a subtle reticular pigment network, and diffuse whitish areas with serrated borders (pseudopods) |
| Shagreen patch | White/yellow structureless areas and reticular vessels with brownish background |
| Vitiligo | Diffuse white structureless area, which is seen as “white glow”, perilesional pigmentation, and residual pigmentation |
| Idiopathic guttate hypomelanosis | White structureless area with pseudopod-like extensions at periphery |
| Pityriasis alba | Ill-defined area with diffuse white scales with subtle pigment network |
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Tuberous sclerosis complex: Review based on new diagnostic criteria. An Bras Dermatol. 2018;93:323-31.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical, histopathological and ultrastructural characteristics of naevus depigmentosus. Clin Exp Dermatol. 2008;33:400-5.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopic patterns of genodermatoses: A comprehensive analysis. Biomedicines. 2023;11:2717.
- [CrossRef] [PubMed] [Google Scholar]
- Simultaneous occurrence of neurofibromatosis type 5 and clustered incomplete tuberous sclerosis. J Eur Acad Dermatol Venereol. 2007;21:1278-80.
- [CrossRef] [PubMed] [Google Scholar]
- Uncoupling of ER/mitochondrial oxidative stress in mTORC1 hyperactivation-associated skin hypopigmentation. J Invest Dermatol. 2018;138:669-78.
- [CrossRef] [PubMed] [Google Scholar]
- Nevus depigmentosus following the Blaschko lines with the robustly activated mTOR pathway. J Eur Acad Dermatol Venereol. 2020;34:e410-2.
- [CrossRef] [PubMed] [Google Scholar]





