Translate this page into:
Coexistence of mixed vaginitis with cervicitis: A changing trend

*Corresponding author: Dr. Swastika Suvirya, Department of Dermatology, Venereology and Leprosy, King George’s Medical University, Lucknow, Uttar Pradesh, India. swastika.p@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Agarwal A, Rawat D, Gupta P, Suvirya S. Coexistence of mixed vaginitis with cervicitis: A changing trend. CosmoDerma. 2024;4:143. doi: 10.25259/CSDM_151_2024
Dear Sir,
A 34-year-old married female presented to the dermatology outdoor department with itching in the genital region along with minimal whitish vaginal discharge for a duration of two years. The discharge had increased over the last two months. The patient had no history of fever, lower abdominal pain, dysuria, or dyspareunia. She reported no history of vesicles, condom use, or chemical douching. The patient’s partner was asymptomatic. The patient and his partner both had been previously treated by gynecologists with acyclovir, Kit-5 (Tab. Acyclovir 400 mg TDS for 7 days), Kit-6 (Tab. Cefiximine 400 mg OD stat + Tab. Metronidazole 400 mg BD for 14 days + Cap. Doxycycline 100 mg BD for 14 days), Kit-1 (Tab. Azithromycin 1 g OD stat + Tab Cefixime 400 mg OD stat), and combination of steroids and antifungal cream all without relief. On clinical examination, the patient had a laxed perineum, and the vaginal examination revealed two types of discharge: A curdy white discharge [Figure 1a-orange arrow] and a thin homogeneous white discharge [Figure 1a-blue arrow]. A per speculum, examination also showed copious homogeneous thin white discharge, from the cervix [Figure 1b]. On examination, the vaginal pH was 5.5. Potassium hydroxide mount and whiff test were negative, but culture from curdy white vaginal discharge showed growth of Candida albicans (>10 Cfu) [Supplementary Figure 1]. Gram staining of the thin whitish vaginal and cervical discharge revealed abnormal vaginal flora with minimal Gram-positive bacilli (score3), plenty of curved Gram-negative bacilli 1–4 (score1), and numerous gram-negative coccobacilli >30 (score 4) per oil immersion field which gave a total Nugent score as 8. Multiple clue cells (>20%) were also visible on the gram stain [Figure 2a] and Papanicolaou stain [Figure 2b]. A polymerase chain reaction test to rule out chlamydia and herpes simplex from cervical discharge was performed and came out to be negative. Routine investigations to rule out other potential underlying condition were all within normal limits. After discussing with the obstetrics department, the patient was eventually diagnosed as a case of bacterial vaginosis (BV) with cervicitis and vulvovaginal candidiasis (VVC). Hence, she was prescribed fluconazole 150 mg daily for seven days and then weekly, and a combination of clotrimazole (100 mg) and clindamycin (100 mg) suppositories for seven days. At one-month follow-up, the patient reported a profound improvement in itching and discharge [Figure 3].
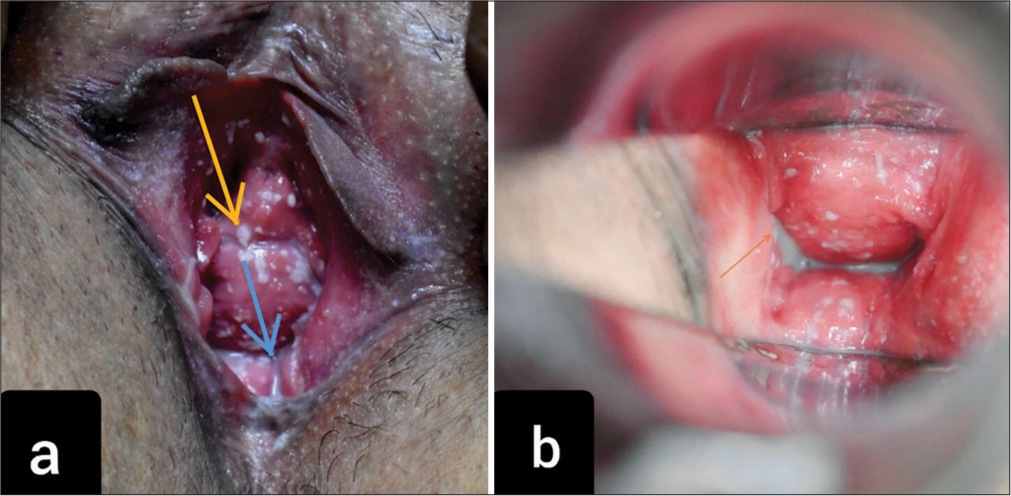
- (a) Curdy white discharge in vagina (orange arrow) and thin homogenous white discharge (blue arrow). (b) Copious thin white homogenous discharge in cervix (orange arrow).
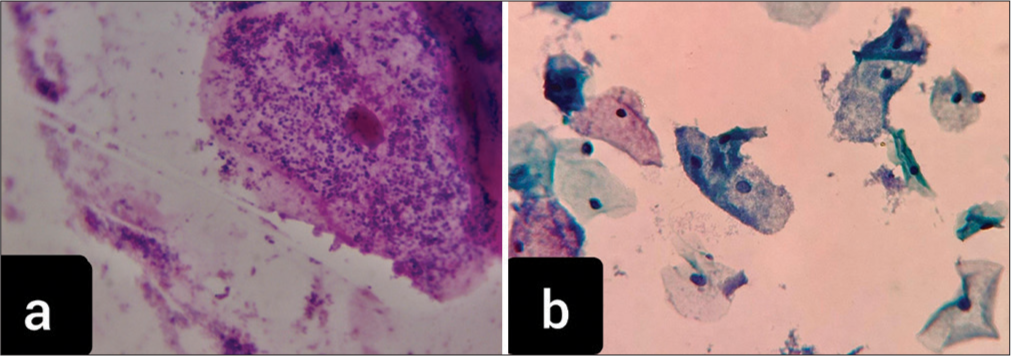
- (a) Gram stain: Clue cells (coating of bacteria over vaginal epithelial cells with loss of cellular border) at a magnification of ×1000. (b) Papanicolaou stain: Smear showing clue cells, characteristic of bacterial vaginosis at a magnification of ×400.

- Resolution of vaginal discharge at follow-up of 1-month.
Mixed vaginitis is the simultaneous presence of at least two types of vaginitis, leads to an abnormal vaginal milieu, and causes atypical symptoms.[1] The frequency of mixed vaginitis ranges from 4.44% to 35.06%, with VVC plus BV being the most prevalent form.[2] The pathogenesis involves multiple microorganisms forming mixed biofilms, embedded in an extracellular matrix,[3] which are responsible for enhancing their drug resistance and evading the host immune response.[1] Cervicitis may occur in women with BV, even without chlamydial or gonococcal coinfection. As we know that the normal vaginal flora is lactobacillus species, some of which are known to produce hydrogen peroxide (H2O2), which is toxic to organisms that either produce little or no H2O2-scavenging enzymes (e.g., catalase).[4] Moreover, BV may lead to the depletion of vaginal mucins, which may further make the mucosa of the vagina and cervix vulnerable. Thus, lack of H2O2-producing lactobacilli and mucin depletion likely contributes to the development of cervicitis in such cases as ours.[5].
Marrazzo et al., in their study on 424 women suffering from BV, found that 15% of the patients had cervicitis too.[5] Similarly, Paavonen et al., in their study on the etiology of cervical inflammation, found an association between mucopurulent cervicitis and Gardnerella vaginalis.[6] Few other researchers too have found a link between BV and cervicitis that is not dependent on concurrent gonococcal and chlamydial infections.[7,8] There are a few studies showing the association of BV and cervicitis but case reports or studies showing a co-occurrence of mixed vaginitis and cervicitis are lacking. To conclude, we should broaden our perspective when encountering cases of BV to also consider the possibility of cervicitis. This approach differs from traditional teachings, which typically identify BV solely as a cause of vaginosis. Moreover, when encountering vaginal discharge, recognizing the potential for mixed infections becomes crucial. This also underscores the importance of a thorough speculum examination, even within a dermatology setting, in cases with vaginal discharge.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Supplementary Figure 1 available on:
Financial support and sponsorship
Nil.
References
- Recent advances in presentation, diagnosis and treatment for mixed vaginitis. Front Cell Infect Microbiol. 2021;11:759795.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of bacterial vaginosis and vulvovaginal candidiasis mixed infection in a Southeastern American STD clinic. Sex Transm Dis. 2011;38:672-4.
- [CrossRef] [PubMed] [Google Scholar]
- Comparative transcriptomic analysis of Gardnerella vaginalis biofilms vs. planktonic cultures using RNA-seq. NPJ Biofilms Microbiomes. 2017;3:3.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of hydrogen peroxide-producing Lactobacillus species in normal women and women with bacterial vaginosis. J Clin Microbiol. 1989;27:251-6.
- [CrossRef] [PubMed] [Google Scholar]
- Risk factors for cervicitis among women with bacterial vaginosis. J Infect Dis. 2006;193:617-24.
- [CrossRef] [PubMed] [Google Scholar]
- Etiology of cervical inflammation. Am J Obstet Gynecol. 1986;154:556-64.
- [CrossRef] [PubMed] [Google Scholar]
- Risk factors for and relationship between bacterial vaginosis and cervicitis in a high risk population for cervicitis in Southern Iran. Eur J Epidemiol. 2001;17:89-95.
- [CrossRef] [PubMed] [Google Scholar]
- Bacterial vaginosis as a risk factor for upper genital tract infection. Am J Obstet Gynecol. 1997;177:1184-7.
- [CrossRef] [PubMed] [Google Scholar]





