Translate this page into:
Circinate balanitis: Clinical and dermoscopic features

*Corresponding author: Neetu Bhari, Department of Dermatology and Venereology, All India Institute of Medical Sciences, New Delhi, India. drntbhari@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Gaurav V, Kumari L, Jain A, Bhari N. Circinate balanitis: Clinical and dermoscopic features. CosmoDerma. 2024;4:54. doi: 10.25259/CSDM_34_2024
A 45-year-old male presented to the sexually-transmitted diseases clinic with asymptomatic genital lesions for seven days. He denied any high-risk sexual behaviors or any other systemic symptoms. He did not take any regular medication, and his medical history was unremarkable. On physical examination, erythematous, well-defined papules and coalescent annular plaques, with white raised polycyclic margins were observed on the glans penis [Figure 1]. Ophthalmological and musculoskeletal examination did not reveal any abnormality. Dermoscopic examination in polarized mode (AM7115MZT Dino-Lite Edge 3.0 digital microscope) at ×30 magnification revealed regions exhibiting merged, uniform red-dotted vessels against an erythematous backdrop [Figure 2]. These areas were encircled by discrete as well as clustered, white pustules arranged in both annular and polycyclic configurations. Tzanck smear, Gram stain, and potassium hydroxide mount revealed pus cells without any multinucleated giant cells, organisms or hyphae. Viral markers, including hepatitis B surface antigen, anti-hepatitis C antibodies, human immunodeficiency virus antigen, and serological tests for syphilis (Venereal disease research laboratory and treponema pallidum hemagglutination assay), were non-reactive. Human leukocyte antigen (HLA) B-27 testing was negative. The urine culture was sterile, and the urinary protein creatinine ratio was negative for Chlamydia and Mycoplasma. The stool culture did not grow any pathogenic organisms. Based on clinical features and dermoscopic findings, the patient was diagnosed with circinate balanitis. The patient was prescribed topical tacrolimus 0.1% cream, resulting in complete resolution within the following 14 days [Figure 3].

- Erythematous, well-defined papules, and coalescent annular plaques, with white raised polycyclic margins over the glans penis.
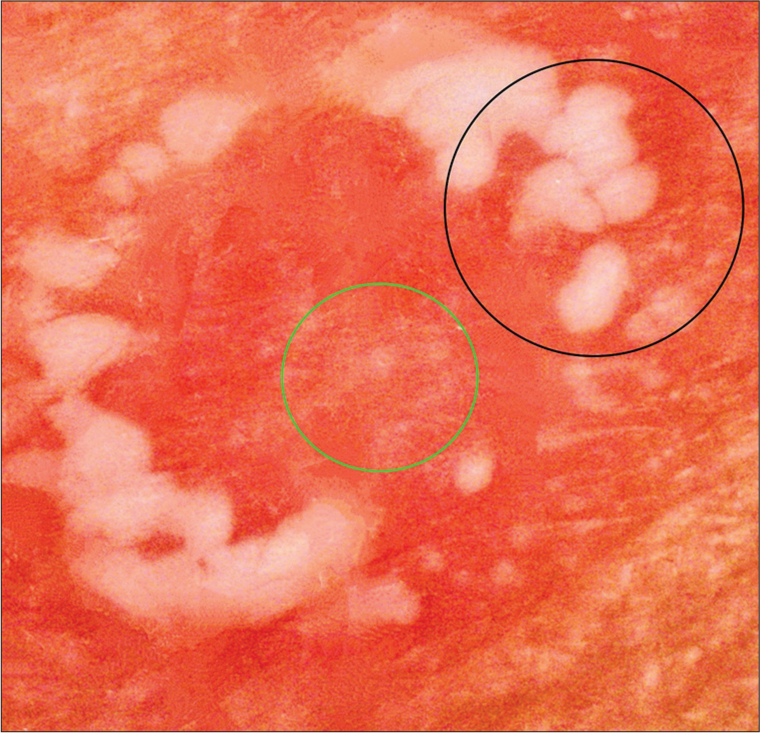
- Dermoscopic examination in polarized mode (AM7115MZT Dino-Lite Edge 3.0 digital microscope) at ×30 magnification showing uniform red dotted vessels against an erythematous backdrop (green circle), encircled by clustered, white pustules arranged discretely as well as in both annular and polycyclic configurations (black circle).

- Resolution of the lesions following treatment with residual erythema.
Circinate balanitis presents as annular erythematous erosive plaques with polycyclic margins on the glans penis and prepuce, commonly associated with reactive arthritis. Reactive arthritis, an inflammatory spondyloarthritis, can be either sexually acquired reactive arthritis or enterically acquired reactive arthritis and is linked to HLA-B27. Circinate balanitis may present independently or alongside other mucocutaneous features of reactive arthritis, including keratoderma blenorrhagicum, circinate balanitis, ulcerative vulvitis, nail dystrophy, oral ulcers, geographic tongue, and conjunctivitis.[1] The dermoscopic observations of annular and polycyclic pustules, dotted vessels, and an erythematous background have been found to correspond with histopathological features such as dermal neutrophilic infiltrates, increased papillary dermal capillaries, and upper dermal capillary dilatation, respectively.[2] However, these findings are not specific to circinate balanitis, as other dermatoses like annular pustular psoriasis may show similar dermoscopic features due to comparable histopathological findings.
The primary approach to treating circinate balanitis typically involves topical corticosteroid therapy, such as hydrocortisone or triamcinolone being commonly utilized. In addition, alternative treatments may include a combination of 10% salicylic acid ointment and hydrocortisone 2.5% cream, oral aspirin, topical calcineurin inhibitors (0.1% tacrolimus or pimecrolimus 1% cream), and a combination of dapsone with calcineurin inhibitors.[3]
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Surface manifestations of Reiter's disease in the male. Br J Vener Dis. 1960;36:36-9.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopy of circinate balanitis. Indian Dermatol Online J. 2021;12:488-9.
- [CrossRef] [PubMed] [Google Scholar]
- Successful use of dapsone for the management of circinate balanitis. Clin Exp Dermatol. 2014;39:333-5.
- [CrossRef] [PubMed] [Google Scholar]





