Translate this page into:
Atypical disseminated hemorrhagic varicella mimicking toxic epidermal necrolysis in an immunocompetent adult

*Corresponding author: Tarun Narang, Department of Dermatology, Post Graduate Institute of Medical Education and Research, Chandigarh, India. narangtarun2012@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Gupta M, Sharma A, Singh S, Narang T. Atypical disseminated hemorrhagic varicella mimicking toxic epidermal necrolysis in an immunocompetent adult. CosmoDerma. 2025;5:54. doi: 10.25259/CSDM_29_2025
Dear Sir,
In recent years, varicella in adults with immune suppression has become increasingly recognized often presenting with greater severity and a higher risk of complications, such as bacterial skin infections, pneumonia, and rare but severe neurological manifestations. Immunocompromised individuals with varicella may require hospitalization, highlighting the importance of preventive measures, including vaccination, to mitigate the risks associated with this viral infection. Hemorrhagic varicella is predominantly reported in immunocompromised individuals due to impaired viral clearance. However, transient immune dysregulation, possibly induced by prior corticosteroid use, may predispose immunocompetent individuals to severe disease manifestations.
Disseminated hemorrhagic varicella is an uncommon but serious complication of varicella, characterized by systemic involvement and severe morbidity. In this report, we describe the case of a young male who presented with disseminated varicella exhibiting an atypical clinical manifestation, highlighting the challenges faced in diagnosis and management.
A 23-year-old male presented to the emergency with a rash accompanied by fever and exertional breathlessness following a 1-day history of aceclofenac tablet intake for abdominal pain. Based on the history of recent drug exposure and the lesional morphology, he was initially managed as a case of toxic epidermal necrolysis (TEN), with supportive treatment and was planned to initiate cyclosporine following dermatology consultation.
His past medical history revealed a history of atopic dermatitis and asthma for which he had been prescribed oral and topical steroids 4 months prior. However, he discontinued their use after 1 month and had no active dermatitis at presentation. There was no history of other comorbidities, prior varicella infection, or recent contact with individuals affected by varicella.
On examination, he had extensive hemorrhagic vesicles, targetoid lesions, necrotic lesions in the inguinal region, conjunctival suffusion, and erythematous papules on the scalp [Figure 1a]. Mucosal examination showed hemorrhagic crusting of the nasal mucosa, erythema with hemorrhagic vesicles on the labial mucosa [Figure 1b], and erosions in the genital mucosa. Further investigations indicated elevated transaminases, acute kidney injury, and thrombocytopenia. Chest radiographs showed interstitial infiltrates consistent with bronchopneumonia, while abdominal ultrasound revealed no abnormalities.
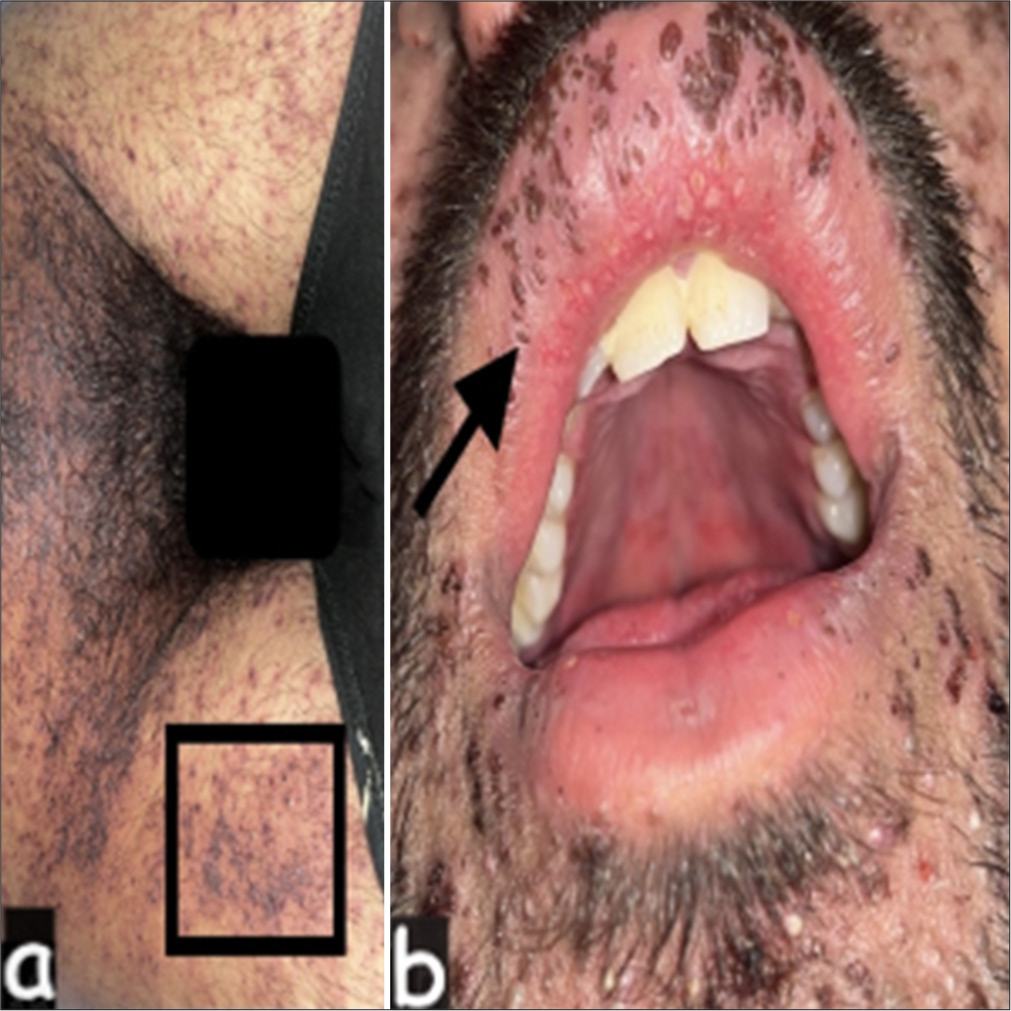
- (a) Extensive hemorrhagic vesicles with necrotic changes, primarily in the inguinal region, suggestive of disseminated hemorrhagic varicella (square). (b) Hemorrhagic crusting in the nasal mucosa and vesicles on the labial mucosa, which can mimic mucosal involvement in Stevens–Johnson syndrome or toxic epidermal necrolysis (arrow).
A Tzanck smear revealed multinucleated giant cells indicative of viral cytopathic effects [Figure 2], raising suspicion of disseminated hemorrhagic varicella. Elevated procalcitonin prompted blood culture, showing Staphylococcus aureus sensitive to ceftriaxone. Screening tests for both primary and secondary immunodeficiency were conducted, and the results were within the normal range. A diagnosis of disseminated hemorrhagic varicella was considered with sepsis, and treatment with tablet valacyclovir, injection ceftriaxone, nebulized saline, oxygen, and paraffin gauze dressings was initiated. After a week of treatment, significant improvement was seen in cutaneous lesions, thrombocytopenia, transaminitis, and respiratory signs and symptoms.

- Tzanck smear showing multinucleated giant cells, a hallmark of viral cytopathic effect, confirming varicella-zoster virus infection.
Hemorrhagic vesicles although common in immunosuppressed patients are rare in typical infection, occurring in only 3.3% of childhood cases.[1] Disseminated varicella infection is known to be preceded by abdominal pain with negative imaging as was seen in our patient.[1] Varicella can also present atypically with distal involvement, resembling the clinical picture of a Steven Johnson syndrome-toxic epidermal necrolysis (SJS-TEN) overlap syndrome. While varicella-associated erythema multiforme and even varicella-induced TEN have been documented, these cases primarily involve children. Differentiating hemorrhagic varicella from TEN is crucial, given the significant overlap in cutaneous manifestations. Unlike TEN, hemorrhagic varicella presents with vesiculobullous lesions in different stages of evolution, lacks a positive Nikolsky sign, and is associated with multinucleated giant cells on Tzanck smear. In addition, real-time polymerase chain reaction for varicella-zoster virus (VZV) DNA can provide a definitive diagnosis in atypical cases.
Hemorrhagic varicella[2] is attributed to endothelial damage caused by VZV, leading to vascular leakage, thrombocytopenia, and disseminated intravascular coagulation. Although traditionally reported in immunocompromised patients, transient immune suppression due to recent corticosteroid use may predispose immunocompetent individuals to severe disease. Given the potential for life-threatening complications, varicella vaccination in adults – especially those with a history of corticosteroid use or chronic dermatological conditions – should be emphasized to prevent severe manifestations.[3]
Varicella typically presents with vesicles on the trunk but can localize to photo-exposed or inflamed areas or exhibit atypical targets,[4] palmoplantar involvement,[5] or gangrenous changes.[6] In immunocompromised individuals, atypical presentations include abdominal pain, delayed skin rash onset, seizures, and elevated enzyme levels.[7] Disseminated varicella complications encompass retinitis, keratitis, central nervous system involvement, and vasculopathy.[8] Considering immunosuppressive use and atopy,[4] recognizing disseminated varicella promptly is crucial to prevent serious complications. Differential diagnosis, especially with Kaposi varicelliform eruption in the setting of atopy, requires careful evaluation.
This case underscores the complexity of disseminated varicella infections in adults, emphasizing the critical need for healthcare providers to accurately differentiate them from other skin conditions for timely intervention and improved prognosis. By doing so, we can ensure the best possible outcomes for patients and provide them with the highest standard of care.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- An observational study of complications in chickenpox with special reference to unusual complications in an apex infectious disease hospital, Kolkata, India. J Postgrad Med. 2013;59:93-7.
- [CrossRef] [PubMed] [Google Scholar]
- Fatal hemorrhagic varicella in a patient with abdominal pain: A case report. BMC Infect Dis. 2020;20:54.
- [CrossRef] [PubMed] [Google Scholar]
- Guidelines for vaccination in normal adults in India. Indian J Nephrol. 2016;26(Suppl 1):S7-14.
- [CrossRef] [Google Scholar]
- Atypical primary varicella rash: Systematic literature review. Acta Paediatr. 2022;111:935-9.
- [CrossRef] [PubMed] [Google Scholar]
- Atypical varicella with palm and sole involvement. Int J Dermatol. 2002;41:903-5.
- [CrossRef] [PubMed] [Google Scholar]
- Gangrenous chickenpox with atypical clinical and histopathological findings. Dermatopathology (Basel). 2018;5:38-40.
- [CrossRef] [PubMed] [Google Scholar]
- Different clinical presentations and outcomes of disseminated varicella in children with primary and acquired immunodeficiencies. Front Immunol. 2020;11:595478.
- [CrossRef] [PubMed] [Google Scholar]
- Disseminated varicella with multiorgan failure in an immunocompetent adult. J Med Virol. 2009;81:747-9.
- [CrossRef] [PubMed] [Google Scholar]





