Translate this page into:
A study on clinicodemographical profile of patients availing the teledermatology service at a tertiary care center in Northeast India

*Corresponding author: Anita Marak, Department of Dermatology and STD, North Eastern Indira Gandhi Regional Institute of Health and Medical Sciences, Shillong, Meghalaya, India. anita.marak@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Marak A, Verma S, Sakshi K. A study on clinicodemographical profile of patients availing the teledermatology service at a tertiary care center in Northeast India. CosmoDerma. 2024;4:67. doi: 10.25259/CSDM_54_2024
Abstract
Objectives:
Delivery of patient care services has drastically evolved where teledermatology specifically has brought about a paradigm shift in our day-to-day practice and has been increasingly utilized since the pandemic era. Keeping this in mind, we conducted a study to evaluate the clinical and demographical profile of patients availing teledermatology service in a tertiary care center in North East India.
Materials and Methods:
This was a retrospective study where the database of patients utilizing the teledermatology facility was analyzed for a period of one year (January 2022–March 2023).
Results:
A total of 74 patients were included in the study, and the data was analyzed based on the store and forward approach. There was a female preponderance with a male: female ratio of 1:2.5. Most of the patients (88%) hailed from an urban background. The highest frequency of users for this service were those aged between 20 and 30 years (35%). The median age was 24 years. The pediatric population comprised 4% of the cases. The diagnosis was possible for 61 (82.4%) cases. The four most common conditions encountered were acne (31.8%), eczematous disorders (18%), melasma (14.8%), and superficial fungal infections (13.3 %). Chronic cases (74%) exceeded the acute cases (26%) in numbers. In the remaining cases where diagnosis was not possible (18%), they were asked to come for a face-to-face consultation; however, none of these patients turned up. In contrast, only 4% of the patients where a diagnosis was possible opted for a re-consultation through teledermatology and none chose to visit the clinic.
Conclusion:
Through this study, we identified patterns in the utilization of teledermatology concerning commonly encountered dermatoses, as well as the age and demographics of patients engaging in teledermatology. This information can be instrumental in the future to pinpoint areas where teledermatology could be more effectively employed.
Keywords
Teledermatology
Store and forward approach
Telemedicine
INTRODUCTION
Telemedicine can be defined as a contemporary technology that provides remote health-care service. Dermatology, a field heavily reliant on visual assessment, is particularly well suited for this type of health-care approach. Teledermatology has served multiple functions: Health-care professionals can utilize this technology to offer clinical assistance to patients, monitor patient well-being, engage in consultations with fellow health-care providers, and grant patients access to educational materials.
Various models and modes of delivery of such services have been categorized based on the nature of the involved actors.[1] The categories of teledermatology are described in Table 1 while Table 2 depicts the different delivery methods of teledermatology.[2]
| Primary TD | This involves direct communication between the patient and GP, nurses, or dermatologists. It serves as a direct channel for initial diagnosis and referral. |
| Secondary TD | This model involves indirect communication between the patient and a specialist. The patient consults with a nurse or GP, who then communicates with the specialist (provider) to seek advice |
| Tertiary TD | This involves a “second” opinion sought among specialists, typically between dermatologists and a dermatologist with a specific specialization. |
| Patient- assisted TD | In this model, the patient communicates with a health-care professional, often for follow-up or the monitoring of skin conditions. |
| Direct-to-consumer TD | The patient takes the initiative by accessing health-care providers directly through personal devices such as smartphones, laptops, or tablets. |
GP: General practitioners, TD: Teledermatology
| RT video consultation (live interactive) | This method utilizes live video conferencing, offering the advantage of providers asking clarifying questions that can provide additional insights to the seeker |
| Asynchronous SAF | In this modality, clinical, dermoscopic, and other specialized images are transmitted for consultation. The provider reviews and responds at a time convenient for them. |
| Hybrid | This modality integrates the aforementioned approaches, combining elements of both RT and asynchronous store-and-forward modalities |
RT: Real-time, SAF: Store-and-forward
Thus, using the store-and-forward pattern,[1,3] this study aimed to discern how teledermatology is being utilized, focusing on the patterns related to patient clinical and demographic characteristics.
MATERIALS AND METHODS
This study was conducted after ethical clearance from the institute. Data of patients was analyzed for one year (January 2022–March 2023). Demographic details of the patients, clinical signs and symptoms, diagnosis, differential diagnosis, and whether diagnosis could be made by image were collected and analyzed.
RESULTS
A total of 74 patients were included in this study.
Demographic details
While assessing the patients according to age groups in this research, our patients ranged from youngest being 6 months to oldest 88 years of age, and the highest frequency of users for this service was those aged between 20 and 30 years (35%). The median age was 24 years. Conversely, the number of older (>60 years) patients was notably lower, as indicated in the provided chart. Our findings indicate that only 4% of the patients were from the pediatric population and 2.7% were from the elderly population. The age-wise distribution of the patients is represented in Figure 1.
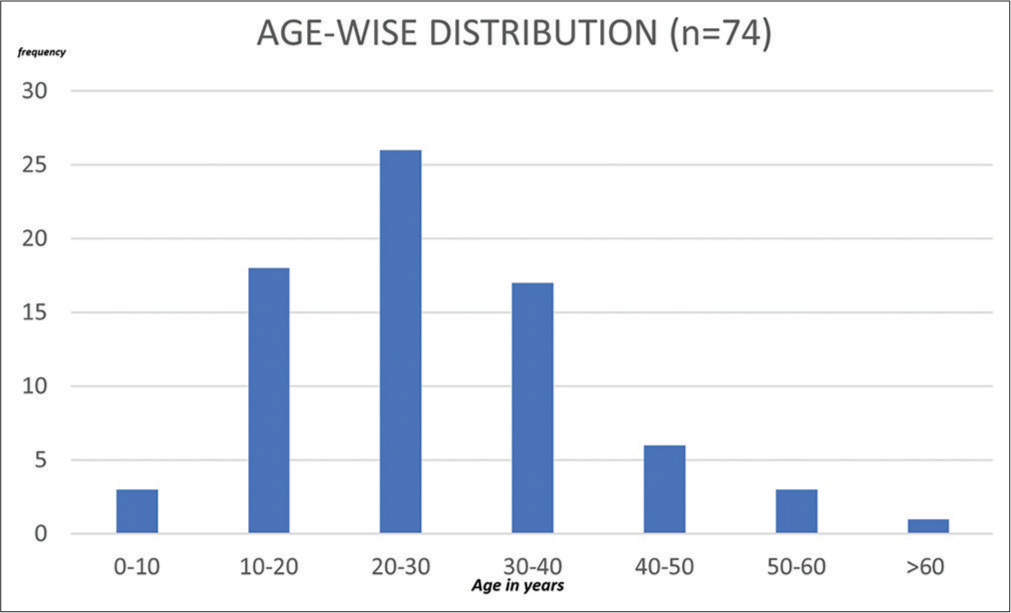
- Age-wise distribution.
Females outnumbered males with a M: F ratio of 1:2.5.
The majority of the individuals (about 88%) were from urban areas, whereas a mere 12% hailed from rural areas.
Clinical characteristics
A clinical diagnosis could be established for 61 individuals (making up 82% of the total). However, the condition of the remaining 13 patients (18%) could not be diagnosed.
Among the 61 patients in whom a diagnosis was attainable, acne (32.8%) followed by eczema (18%), melasma (14.8%), and superficial fungal infections (13.3%) were the most common diagnoses made. The various diagnoses made in our study are represented in Figure 2.
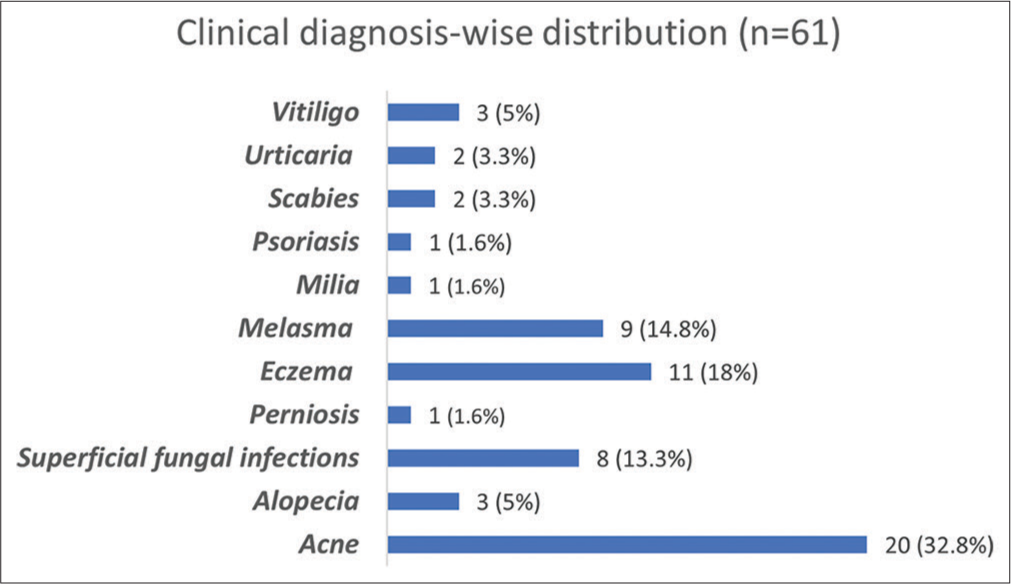
- Graph depicting clinical case-wise distribution.
Of the three pediatric cases encountered, the diagnosis could not be made in one, whereas the other two were identified as scabies and vitiligo, respectively.
The diagnosis was inconclusive for one of the two patients from the elderly population (>60 years), whereas the other was diagnosed with melasma.
Patients where a diagnosis was not possible were asked to follow up for a visit in the outpatient department (OPD); however, none of them turned up.
In terms of old versus new cases, the proportion was 1:73.
When considering the duration of the illness, we found that 74% of the cases presented to us were chronic (duration >6 weeks) and 26% were acute. Different illnesses by duration are represented in Table 3.
| Acute | Chronic |
|---|---|
| Acne-7 | Acne-13 |
| Eczema-3 | Eczema-9 |
| Superficial fungal infections-4 | Superficial fungal infections-4 |
| Perniosis-1 | Melasma-9 |
| Scabies-1 | Scabies-1 |
| Vitiligo-3 | |
| Urticaria-2 | |
| Psoriasis-1 | |
| Alopecia-3 | |
| Milia-1 |
Regarding the choice of follow-up of the patients where a diagnosis was possible, either by teleconsultation or face-to-face visit, merely 4% of them opted for a follow-up through teleconsultation while none of the patients preferred in-person consultation.
DISCUSSION
Many published teledermatology articles have typically centered around a single disease, such as melanoma,[4-6] acne,[7,8] or a specific class of diseases, such as malignant tumors.[9-11] One study from north India by Tuknayat et al.[12] had a more comprehensive approach, addressing a range of dermatological conditions. Our study marks the pioneering effort of its kind in northeast India.
A noteworthy observation was the age-related utilization pattern, where 44.5% of individuals seeking teledermatology services fell within the young adult age group, with a peak occurring between 20 and 30 years of age. This trend can potentially be attributed to the higher familiarity with using technology, having easier access to the Internet, and willingness to use the facility and share digital images in younger adults, compared to both older individuals and those who are even younger, leading to a variance in utilization patterns.
In a study from São Paulo, Giavina-Bianchi et al.[13] reported that they found the peak age of utilization to be 60–69 years. This suggests that the elderly population in Western regions may be more adept at using technology than their counterparts in our demographic. There can be many barriers that limit the use of modern telecommunication techniques in the elderly; however, certain measures can be adopted to maximize engagement in them. These include a brief demonstration video or screenshots entailing step-by-step procedure on how to avail the service. For those without Internet/smartphone access, telephone-only encounters can still be effective for initial communication.
Similarly, the variation in patient statistics concerning urban and rural distribution can also be attributed to factors such as limited awareness and accessibility of teleconsultation services among the rural population, especially considering the terrain of the Northeast region where Internet facilities are limited.
However, this observation also underscores the potential for the growth of teledermatology in rural areas. The greater accessibility of teledermatology can benefit more patients, especially considering the limited number or unavailability of dermatologists in such regions.[14]
Out of the 74 patients who were assessed, a diagnosis was achievable for 61 of them. However, factors such as poor quality of the images, insufficient clinical information from patients, and lack of adequate history taking by the health-care provider in the store-and-forward approach contributed to the inability to make a clinical diagnosis in about 13 patients (18%).
The effectiveness of each telemedicine platform is contingent upon factors such as the specific medical condition, image quality, and the proficiency of the health-care provider.[14] Furthermore, accessing telemedicine is influenced by both network connectivity and socioeconomic status.[15] Oakley and Rennie[16] conducted a study involving 384 cases, a diagnosis was possible for 96% of the cases whereas 4% remained without a definitive diagnosis.
The patients where a diagnosis could not be made were asked to review either in the OPD or for a face-to-face visit but none of these patients came back for follow-up. In addition, out of all the patients on whom the diagnosis was possible, only 3 patients (4.9%) followed up for a re-consultation through teledermatology and none for a face-to-face visit.
This could be explained by different reasons; achievement of clinical improvement, the skin condition was not affecting the patient to the extent wherein they felt the need for an in-person visit or patients were reluctant to follow up. However, in a study conducted by Oakley and Rennie,[16] the attendance rate for new patients was 86.6% and for follow-ups, it was 78.9% which was much higher than our study. Adherence to follow up can be increased by ensuring that there is a provision for a reminder text message, email, or call regarding the follow-up. In addition, a separate counter for registration of in-person visits for such patients will reduce the time of consultation, especially for those who are hesitant to come due to long waiting hours.
Regarding the distribution of cases based on diagnosis, the most common was acne (31.8%) followed by eczematous disorders (18%), melasma (14.8%), and superficial fungal infections (13.3%). In a study from North India by Tuknayat et al.,[12] infections/infestations (29.5%), eczematous disorders (22.9%), and acne (12.6%) comprised the three most common conditions encountered. We can observe a discernible trend concerning the types and frequencies of various clinical conditions commonly encountered through teleconsultation. This data can potentially serve as valuable insight for future endeavors in triaging conditions through teleconsultation, aiming to minimize in-person visits for diseases that can effectively be managed online through teledermatology.
Another observation was that most of the conditions that were presented to us were chronic in nature, even in the eczematous group. Acne, eczemas, and superficial fungal infections were the three most common categories in both the acute and chronic groups, but the number of patients in the above-mentioned categories was higher in the chronic group as represented in Table 3. This discordance between acute and chronic groups could be explained by the fact that the patients with acute dermatological conditions preferred in-person visits because of their symptomatic nature contrary to the patients with chronic disorders, who opted for teleconsultation.
Future prospect in teledermatology
Although we did not find any skin malignancies in our study, teledermatology can still be a valuable tool for screening pre-malignant and malignant skin conditions. This can be achieved by setting up dedicated telemedicine units in peripheral areas, equipped with dermatoscopy, which can then transmit images to tertiary care centers. Alternatively, artificial intelligence-based applications can be developed to assist health professionals in the periphery in recognizing malignant skin conditions. Expanding the use of teledermatology and enhancing patient engagement can be achieved by incorporating real-time live video conferencing. Patients with vesiculobullous disorders, connective tissue disorders, and skin cancers, who require regular follow-up for monitoring of their disease, can be encouraged to use the store and forward approach. This would help reduce the need for in-person visits with lower transportation expenses.
Limitations
The study’s sample size was restricted because it was carried out over 1 year, and an extension was not feasible because of the non-availability of patients participating in teledermatology after 2023. The store and forward approach is a simple and user-friendly method of teledermatology. However, it has its own limitations viz a viz real-time video conferencing where making a diagnosis becomes difficult, as seen in our study. In addition, the follow-up of patients for making a diagnosis or monitoring was also not satisfactory with this approach.
CONCLUSION
Through this study, our main purpose was to highlight the various conditions that we encounter in our teledermatology setup at a referral center using the store and forward method and to also see the demography of the patients particularly in the peripheral areas where such services are either not accessible or not utilized to its maximum potential as supported by our study where the majority of the utilizers were from an urban background. Similarly, we also observed that the elderly population in our part of the country is underutilizing this service despite its convenience and easy accessibility. In terms of dermatological conditions, acne, eczematous disorders, melasma, and superficial fungal infections were the most common dermatoses encountered, which can often be managed by primary health-care providers while patients with dermatological conditions that require specialist attention such as autoimmune blistering, connective tissue disorders, hair, nail related dermatoses, and skin cancers were not utilizing this facility at all.
Ethical approval
The research/study was approved by the Institutional Review Board at North Eastern Indira Gandhi Regional Institute of Health and Medical Sciences, number IEC/M11/F15/2023, dated August 07, 2023.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Teledermatology and its current perspective. Indian Dermatol Online J. 2020;11:12-20.
- [CrossRef] [PubMed] [Google Scholar]
- State of teledermatology programs in the United States. J Am Acad Dermatol. 2012;67:939-44.
- [CrossRef] [PubMed] [Google Scholar]
- Teledermatology: Clinical case profiles and practical issues. Indian J Dermatol Venereol Leprol. 2009;75:32-5.
- [CrossRef] [PubMed] [Google Scholar]
- Teledermatology: Current indications and considerations for future use. Arch Dermatol Res. 2021;313:11-5.
- [CrossRef] [PubMed] [Google Scholar]
- Melanoma detected through teledermatology versus in-person visits. Telemed J E Health. 2024;30:e1192-6.
- [CrossRef] [PubMed] [Google Scholar]
- Teledermatology in the diagnosis of melanoma. J Telemed Telecare. 2014;20:18-23.
- [CrossRef] [PubMed] [Google Scholar]
- Assessing acne severity: Teledermatology versus face to face consultations during the COVID-19 pandemic. J Clin Aesthetic Dermatol. 2023;16:30-4.
- [Google Scholar]
- Comparing acne follow-up: Teledermatology versus outpatient dermatology visits. Dermatol Online J. 2015;26:13030/qt1424r02m.
- [CrossRef] [Google Scholar]
- Teledermatology applications in skin cancer diagnosis. Dermatol Clin. 2017;35:559-63.
- [CrossRef] [PubMed] [Google Scholar]
- Smartphone teledermoscopy referrals: A novel process for improved triage of skin cancer patients. Acta Derm Venereol. 2015;95:186-90.
- [CrossRef] [PubMed] [Google Scholar]
- Teledermoscopy in high-risk melanoma patients: A comparative study of face-to-face and teledermatology visits. Acta Derm Venereol. 2016;96:779-83.
- [Google Scholar]
- Clinical profile and diagnostic accuracy of patient-submitted photographs in teledermatology. J Clin Aesthetic Dermatol. 2023;16:21-5.
- [Google Scholar]
- Teledermatology reduces dermatology referrals and improves access to specialists. EClinicalMedicin. 2020;29-30:100641.
- [CrossRef] [PubMed] [Google Scholar]
- Teledermatology: A possible reality in rural India. Int J Dermatol. 2015;54:375-6.
- [CrossRef] [PubMed] [Google Scholar]
- Recent trends in teledermatology and teledermoscopy. Dermatol Pract Concept. 2018;8:214-23.
- [CrossRef] [PubMed] [Google Scholar]
- Retrospective review of teledermatology in the Waikato, 1997-2002. Australas J Dermatol. 2004;45:23-8.
- [CrossRef] [PubMed] [Google Scholar]






