Translate this page into:
Dermoscopy of cutaneous loxoscelism

*Corresponding author: Aravind Sivakumar, Department of Dermatology, Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry, India. aravinddermat@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sivakumar A, Monisha GA. Dermoscopy of cutaneous loxoscelism. CosmoDerma. 2025;5:52. doi: 10.25259/CSDM_27_2025
A woman in her forties presented with a painful, reddish lesion on her left thigh, appearing 2 days after an alleged spider bite. Initially, a painful erythematous papule, the lesion evolved into a diffuse rash with a central violaceous macule, surrounded by pallor, reflecting the “red, white, and blue” sign, indicative of cutaneous loxoscelism [Figure 1a]. Dermoscopy (DL5 dermatoscope, polarized mode) of the central macule revealed a triphasic appearance: A central pale edema (ischemic zone), a cyanotic ring (thrombosis), and an erythematous ring (vasodilation) [Figure 1b]. A diagnosis of loxoscelism was confirmed with the history, examination findings, and dermoscopy. The patient was treated conservatively with analgesics and antibiotics, showing improvement at 1-week follow-up.
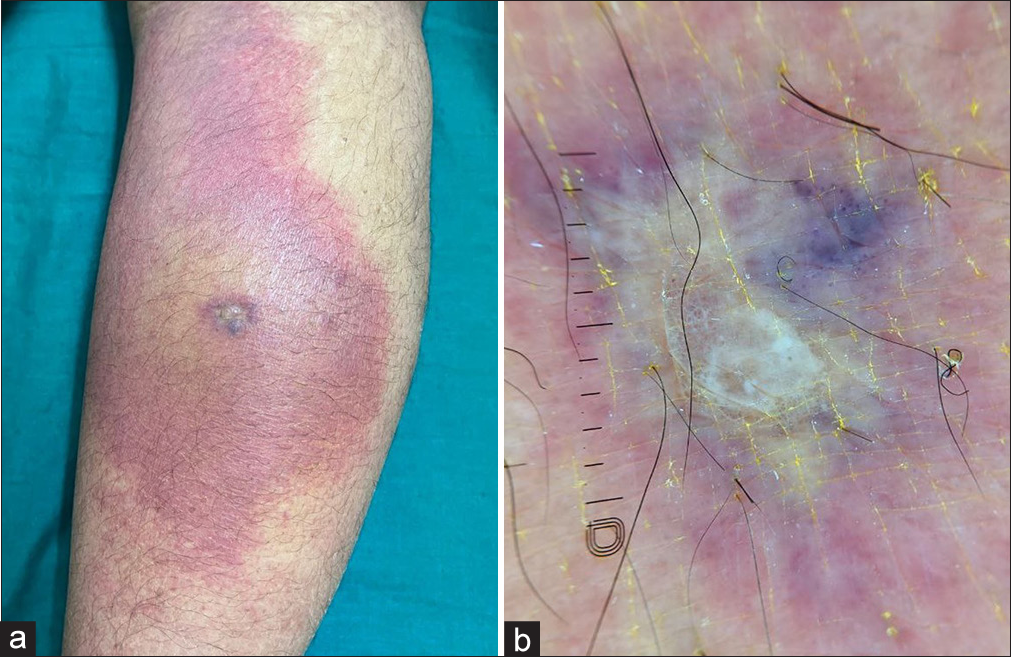
- (a) The characteristic “red, white and blue sign” of cutaneous loxoscelism showing central dusky area, with ring of pallor and peripheral spreading erythema. (b) Dermoscopy (DermLite DL5, polarized mode, ×10 magnification) showing central pale edema, with surrounding cyanosis and peripheral erythema (dermoscopic red, white, and blue sign).
Loxoscelism is caused by spiders from the Sicariidae family (e.g., Loxosceles reclusa). These nocturnal, defensive spiders typically bite in concealed areas, such as the thigh or trunk. The bite site, initially painless, becomes painful and develops the characteristic “red, white, and blue” sign due to central necrosis with surrounding vasoconstriction and peripheral ring of vasodilation. This may progress to eschar formation due to mediators such as sphingomyelinase D, lipase, and hyaluronidase, leading to necrotic arachnidism.
Differential diagnoses include scrub typhus, cutaneous anthrax, ecthyma gangrenosum, and purpura fulminans. Rarely, systemic toxicity may cause myalgia, headache, hemolytic anemia, thrombosis, disseminated intravascular coagulation, and acute generalized exanthematous pustulosis.
Treatment is primarily conservative, with rest, ice, compression, elevation, analgesics, antibiotics, and wound care. Severe cases may require dapsone and systemic steroids.
Thus dermoscopy can aid in the early diagnosis of spider envenomation, ensuring timely and appropriate management.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.





