Translate this page into:
Clinical approaches in vogue for combination therapies for acne and post-inflammatory hyperpigmentation – A comprehensive review

*Corresponding author: Oluwatosin Christiana Adebusoye, Department of Life Sciences and Education, University of South Wales, Cardiff, United Kingdom. oluwatosinalade228@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Adebusoye OC, Srivastava G. Clinical approaches in vogue for combination therapies for acne and post-inflammatory hyperpigmentation – A comprehensive review. CosmoDerma. 2025;5:11. doi: 10.25259/CSDM_174_2024
Abstract
Acne and post-inflammatory hyperpigmentation (PIH) are prevalent dermatological conditions that significantly impact young individuals, especially those with darker skin tones. Effective management of these conditions requires a comprehensive approach that integrates topical, systemic, and procedural therapies. The evaluation of the data from multiple clinical studies and dermatological reviews revealed the superior efficacy of combination therapies for acne and PIH. The studies incorporated the analysis of the effectiveness of topical agents such as retinoids (tretinoin and adapalene) and hydroquinone, systemic treatments such as antibiotics and hormonal agents, and procedural interventions including laser therapy and chemical peels. Topical therapies showed a significant efficacy in reducing acne lesions and PIH and emphasized on a superior response in patients on combination therapies when compared to monotherapy. Systemic treatments are very effective for severe acne and aid indirectly in mitigating PIH. Procedural therapies enhance treatment efficacy by targeting pigmented cells and stimulating skin regeneration. The integration of multiple treatment modalities addresses the complex pathophysiology of acne and PIH in a better way. Topical retinoids accelerate cell turnover and reduce inflammation, while hydroquinone inhibits melanogenesis. Combining these agents with systemic treatments or procedural interventions maximizes therapeutic benefits. Personalized treatment plans, tailored to individual skin types and conditions, are crucial for optimizing outcomes. Combination therapy thus represents a robust approach to managing acne and PIH, offering enhanced efficacy through synergistic effects. Further research in the light of present work is needed to refine these strategies and develop new formulations that address both cosmetic and biomedical aspects of PIH.
Keywords
Acne
Post-inflammatory hyperpigmentation
Combination therapy
Retinoids
Hydroquinone
Laser therapy
Chemical peels
Personalized treatment
INTRODUCTION
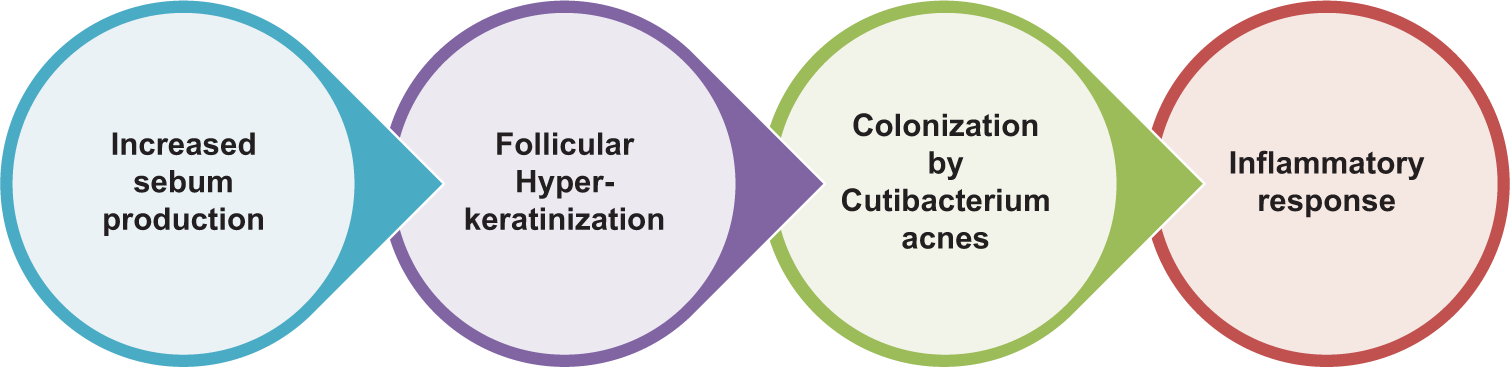
Acne vulgaris, commonly known as acne, is a chronic inflammatory skin condition characterized by blackheads, whiteheads, pimples, oily skin, and residual scarring. It predominantly affects areas of the skin with a relatively high number of oil glands, including the face, upper part of the chest, and back. The pathogenesis of acne involves four primary factors, namely increased sebum production, hyper-keratinization, microbial colonization of the skin (particularly with Cutibacterium acnes), and inflammation. The epidemiology of acne indicates that it is a global concern, affecting approximately 85% of young adults aged 12–25 years.[1] However, its prevalence is not limited to adolescents, as adults, especially women, can experience acne with varying severity and persistence.[2] Post-inflammatory hyperpigmentation (PIH) is more common in individuals with darker skin tones and occurs when an inflammatory disorder causes the skin to produce excess melanin.[3] The relationship between acne and PIH is significant because the inflammatory process of acne can lead to hyperpigmentation, especially if acne lesions are picked or squeezed.[4]
The clinical challenge lies in the dual problem of treating acne effectively while preventing or managing PIH. It is compounded by the varied skin types, tones, and individual responses to treatment, making a “one-size-fits-all” approach ineffective. The complexity of simultaneously managing these conditions necessitates a comprehensive understanding of their pathophysiology, the impact of various treatments on both conditions and the importance of individualized patient care.
COMBINATION THERAPIES
Combination therapy has become a cornerstone in the management of acne and PIH due to its multifaceted benefits. This approach involves the simultaneous use of multiple therapeutic agents or modalities, each targeting different aspects of the conditions, to enhance treatment efficacy, reduce the potential for resistance, and address various pathogenic factors simultaneously. Using a combination of treatments, such as retinoids and benzoyl peroxide, each targeting specific pathogenic factors, the overall efficacy of treatment improves significantly compared to monotherapy. For instance, retinoids help normalize keratinization and reduce inflammation, while benzoyl peroxide exhibits potent antimicrobial activity against C. acnes.[5] Similarly, PIH can be more effectively managed with combination therapy. Using agents like hydroquinone to inhibit melanin synthesis, along with retinoids to enhance skin cell turnover, can lead to faster and more noticeable improvements in pigmentation.[6] When antibiotics are used as monotherapy, C. acnes can develop resistance, rendering the treatment less effective over time. Combination therapy mitigates this risk by incorporating non-antibiotic agents that have different mechanisms of action. For example, combining topical antibiotics with benzoyl peroxide not only enhances the antibacterial effect but also reduces the likelihood of developing antibiotic-resistant strains of bacteria.[5]
Combination therapy allows for a more holistic approach to treatment by addressing multiple symptoms concurrently. For instance, in severe acne cases, combining oral isotretinoin, which reduces sebum production and has anti-inflammatory properties, with topical treatments can provide both immediate and long-term benefits.[7] For PIH, integrating treatments like chemical peels with topical agents can improve skin texture, reduce pigmentation, and enhance overall skin appearance.[8] Combination therapy also offers the flexibility to tailor treatment plans to individual patient needs. Patients with different skin types, varying severities of acne, and degrees of PIH can benefit from personalized treatment regimens. For example, a patient with oily skin and moderate acne might benefit from a combination of topical retinoids and salicylic acid peels, whereas a patient with dry skin and severe PIH might require a regimen combining topical hydroquinone and lactic acid peels.[9,10] However, patient adherence to treatment regimens is crucial for achieving optimal outcomes. Combination therapy can be designed to simplify treatment routines, thereby improving patient compliance. Fixed-dose combination products that include multiple active ingredients in a single formulation can reduce the number of applications required, making it easier for patients to stick to their treatment plans, leading to better treatment outcomes and higher patient satisfaction.[11]
Numerous studies have demonstrated the superiority of combination treatments over monotherapies.[6,11] The American Academy of Dermatology guidelines advocate the use of combination therapies involving topical retinoids, antibiotics, and benzoyl peroxide for optimal acne management.[5,6] Acne comprises both inflammatory lesions (like papules and pustules) and non-inflammatory lesions (like comedones). A combination approach can target both types of lesions effectively. Retinoids are particularly effective for non-inflammatory lesions by promoting cell turnover and preventing comedone formation, while anti-inflammatory agents such as benzoyl peroxide or topical antibiotics are more effective against inflammatory lesions.[6,7] Combining treatments can also improve the safety and tolerability of acne and PIH therapies. Using lower doses of each agent, the overall risk of side effects can be reduced while still achieving therapeutic efficacy. For instance, combining topical retinoids with moisturizers or anti-inflammatory agents can mitigate the irritation and dryness often associated with retinoid therapy.[11]
PATHOPHYSIOLOGY OF ACNE
Acne is primarily caused by increased sebum production, abnormal follicular differentiation, proliferation of C. acnes, and an inflammatory response that leads to the formation of comedones and pustules.[12,13] Following inflammatory damage, the melanocytes can respond by producing excess melanin, resulting in hyperpigmented areas. Effective management of these conditions requires a comprehensive understanding of their complex pathophysiology to develop targeted treatment strategies [Figure 1]. Acne is a multifactorial dermatological condition affecting millions worldwide, with a significant impact not only during adolescence but also in adulthood.[14] It is characterized by a variety of lesions, including comedones, papules, and pustules, which can lead to considerable psychological distress.[15] The pathogenesis of acne includes sebum overproduction, abnormal keratinization, microbial colonization, and inflammation. Hormonal fluctuations play a pivotal role, with androgens stimulating sebaceous gland activity and sebum production. This excessive sebum, coupled with dysregulated keratinization within the follicular epithelium, leads to comedo formation, the initial lesion in acne.[14] The proliferation of C. acnes within the lipid-rich environment of the sebaceous follicle further exacerbates acne. This bacterium contributes to the inflammatory milieu by activating toll-like receptors on keratinocytes and monocytes, leading to the release of pro-inflammatory cytokines such as interleukin (IL)-1β, IL-8, and tumor necrosis factor-alpha. The inflammatory response is a double-edged sword, essential for combating microbial infections but also responsible for tissue damage and subsequent PIH.[16] Abnormal shedding of the follicular epithelium results in the formation of a plug, blocking the pilosebaceous unit, and leading to the formation of microcomedones, which can evolve into visible comedones (blackheads and whiteheads). The inflammatory response in acne involves the activation of innate immune mechanisms, including the release of cytokines and chemokines, leading to the recruitment of inflammatory cells (neutrophils and macrophages) to the site of the lesion, resulting in the formation of inflammatory papules, pustules, and nodules.[14,15]
- Pathophysiology of acne.
PATHOPHYSIOLOGY OF PIH
PIH arises from the overproduction or irregular distribution of melanin following cutaneous inflammation. In the context of acne, inflammatory mediators released during the healing process stimulate melanocytes, leading to increased melanin synthesis. Furthermore, inflammation-induced disruption of the basal layer can cause melanin to spill over into the dermis, where it is taken up by macrophages, forming the persistent dark patches characteristic of PIH. The degree of PIH is notably influenced by the initial severity of the acne lesion and the skin’s baseline pigment. Darker skin types are more prone to PIH due to their melanocytes being more reactive to inflammatory stimuli. This heightened responsiveness underscores the importance of adopting a proactive and preventive approach to managing acne in patients with darker skin to mitigate the risk of PIH.[17]
Factors contributing to PIH include inflammatory mediators, hyperactive melanocytes, and skin injury. These factors increase melanin synthesis and deposition, resulting in hyperpigmented patches that persist long after the resolution of the inflammatory lesions.[18] The impact of PIH varies significantly across different skin types, particularly affecting individuals with darker skin tones (Fitzpatrick skin types IV to VI). These skin types naturally have more active melanocytes, which can produce more melanin. Consequently, the hyperpigmentation seen with PIH can be more pronounced and longer-lasting, often significantly affecting the individual’s quality of life due to the visible nature and persistence of discoloration.[19]
The intricate relationship between acne and PIH necessitates a comprehensive approach that addresses both the active lesions and the risk of hyperpigmentation. Current strategies include the judicious use of topical retinoids, which normalize keratinization and possess anti-inflammatory properties, thereby reducing acne lesions and minimizing the risk of PIH.[20] Moreover, advancements in nonpharmacological treatments such as chemical peels and laser therapy offer promising results in both preventing and treating PIH in acne patients.[21,22] Sun protection is also vital to prevent further pigmentation changes triggered by UV exposure.[23] Understanding these underlying mechanisms is crucial for the development of targeted therapies that can effectively address both conditions. As research progresses, the focus is shifting toward personalized medicine, which promises to deliver tailored treatments based on individual patient characteristics, including genetic predisposition, skin type, and specific pathophysiological mechanisms involved in their condition. Such an approach not only aims to improve acne and PIH outcomes but also enhances patient satisfaction and quality of life.[24]
THERAPIES FOR ACNE AND PIH
Pharmacological therapies for acne and PIH involve a range of medications designed to address the complex pathophysiology of these skin conditions. Acne treatments typically focus on reducing sebum production, combating bacterial growth, and alleviating inflammation [Figure 2]. For PIH, pharmacological interventions aim to reduce melanin production and promote even skin tone. Recently, agents such as azelaic acid and tranexamic acid have gained popularity for their effectiveness in treating PIH, offering anti-inflammatory and melanin-inhibiting properties without the harsh side effects of more aggressive treatments.[25,26]
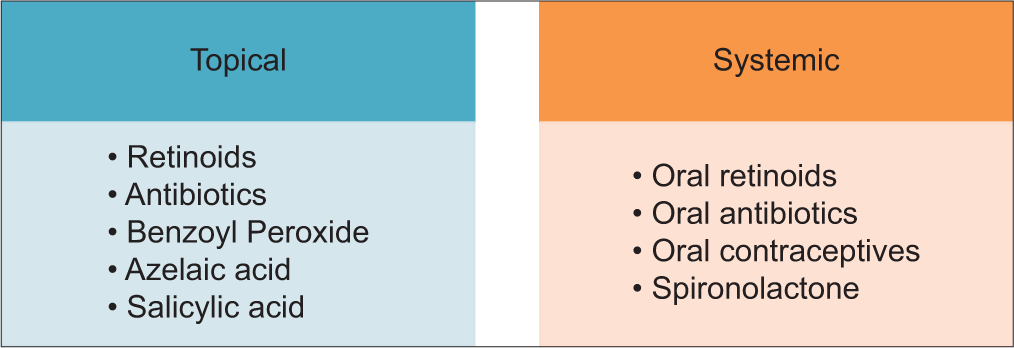
- Treatment options for acne.
TOPICAL THERAPIES
Topical therapies play a pivotal role in the management of acne and PIH, offering targeted treatments that can be applied directly to the affected areas of the skin [Table 1]. These therapies typically include agents that are designed to reduce inflammation, accelerate cell turnover, inhibit melanin production, and kill acne-causing bacteria.[27] Topical therapies often focus on lightening hyperpigmented areas by inhibiting enzymes that produce melanin. Ingredients such as hydroquinone, azelaic acid, vitamin C, niacinamide, and tranexamic acid are gaining popularity for their effectiveness in treating hyperpigmentation without harsh side effects. The choice of topical treatment depends on the severity of the condition, skin type, and the patient’s overall skin health goals. Healthcare professionals often recommend a combination of these therapies to maximize effectiveness and minimize adverse effects, tailoring regimens specifically for each patient’s unique skin characteristics.[28]
| Treatment | Mechanism of Action | Efficacy | Side Effects |
|---|---|---|---|
| Retinoids | Normalize desquamation, reduce inflammation, | High | Irritation, erythema, photosensitivity |
| inhibit comedogenesis | |||
| Benzoyl peroxide | Antimicrobial against C. acnes, keratolytic effects | High | Dryness, peeling, bleaching of hair/clothes |
| Azelaic acid | Antimicrobial, anti-inflammatory, comedolytic | Moderate to high | Mild irritation, itching |
| Topical Antibiotics | Antibacterial action against C. acnes | Moderate | Skin irritation, resistance risk |
| Hydroquinone | Inhibits melanin production | High for PIH | Irritation, ochronosis with prolonged use |
PIH: Post-inflammatory hyperpigmentation, C. acnes: Cutibacterium acnes
Retinoids are a cornerstone in the treatment of acne due to their ability to normalize desquamation, reduce inflammation, and inhibit comedogenesis. They work by binding to nuclear receptors in keratinocytes, promoting cellular differentiation and turnover. This process helps in normalizing the desquamation process, preventing the formation of microcomedones, and reducing inflammation. Clinical trials have consistently demonstrated the efficacy of retinoids in reducing both inflammatory and non-inflammatory acne lesions.[24] However, retinoids can cause skin irritation, including erythema, peeling, and dryness. Patients are advised to use moisturizers and sunscreens to mitigate these side effects. Gradual introduction and using the retinoid every other night initially can help improve tolerability.[20]
Benzoyl peroxide is an antimicrobial agent that generates reactive oxygen species, which have bactericidal effects on C. acnes. It also has mild comedolytic and anti-inflammatory properties, making it effective in both inflammatory and non-inflammatory acne. Its efficacy is enhanced when combined with topical antibiotics or retinoids due to its ability to prevent the development of antibiotic resistance. Patients should be advised to use non-comedogenic moisturizers to alleviate dryness and avoid contact with hair and clothes as it can bleach hair and clothes.[27]
Azelaic acid also exhibits antimicrobial activity against C. acnes and Staphylococcus epidermidis, reduces keratinocyte proliferation, and exhibits anti-inflammatory properties. In addition, it inhibits tyrosinase, an enzyme involved in melanin production, making it effective for PIH. It is particularly beneficial for patients with both acne and PIH due to its dual action. Generally well-tolerated, with mild irritation and itching being the most common side effects, it is a suitable option for patients with sensitive skin who cannot tolerate other topical treatments.[26]
Hydroquinone inhibits the enzyme tyrosinase, thus reducing melanin production, and lightening hyperpigmented areas. It can cause skin irritation and, with prolonged use, may lead to ochronosis, a condition characterized by blue-black pigmentation. It is often recommended for short-term use in PIH.[28]
SYSTEMIC THERAPIES
Oral antibiotics such as tetracyclines (doxycycline and minocycline) and macrolides (erythromycin and azithromycin) are commonly used for moderate-to-severe acne [Table 2]. These antibiotics have both antimicrobial and anti-inflammatory properties. They are effective for inflammatory acne, but their prolonged use can lead to antibiotic resistance. Common side effects include gastrointestinal disturbances, photosensitivity, and potential interactions with other medications. To mitigate resistance, oral antibiotics are often prescribed for a limited duration (typically 2–6 months) and are combined with topical treatments such as benzoyl peroxide or retinoids.
| Treatment | Mechanism of Action | Efficacy | Side Effects |
|---|---|---|---|
| Oral Antibiotics | Antibacterial and anti-inflammatory properties | Moderate to high | Gastrointestinal disturbances, photosensitivity, resistance risk |
| Isotretinoin | Reduces sebum production, normalizes keratinization, anti-inflammatory | Very high | Teratogenicity, dry skin, lips, and eyes, mood changes |
| Hormonal Treatments | Regulate hormonal fluctuations, reduce sebum production | Moderate to high in women | Nausea, weight gain, thromboembolism (OCs); menstrual irregularities, hyperkalemia (Spironolactone) |
OCs: Oral contraceptives
Isotretinoin is a systemic retinoid that is highly effective for severe, recalcitrant acne. It reduces sebum production, normalizes keratinization, and has anti-inflammatory effects.[27,29] It has been shown to induce long-term remission in many patients, significantly reducing the severity and recurrence of acne. However, it has a significant side effect profile, including teratogenicity, mucocutaneous effects (dry skin, lips, and eyes), and potential mood changes. Due to its teratogenic effects, strict pregnancy prevention measures must be followed, including monthly pregnancy tests and the use of two forms of contraception. Regular monitoring of liver function and lipid levels is also required during treatment.[27,30]
Hormonal treatments are particularly beneficial for women with hormonal influences on acne, such as those with polycystic ovary syndrome. Oral contraceptives (OCs) containing estrogen and progestin help regulate hormonal fluctuations, reducing sebum production and improving acne. Spironolactone, an androgen receptor antagonist, reduces androgen-induced sebum production. OCs may cause side effects such as nausea, weight gain, and an increased risk of thromboembolism. Spironolactone may cause menstrual irregularities and hyperkalemia. Hormonal treatments require careful patient selection and monitoring.[29,31]
NON-PHARMACOLOGICAL TREATMENTS
These approaches are particularly significant in dermatology, where they include various procedures and lifestyle adjustments aimed at improving skin health and appearance. These treatments are often used in combination with each other or with pharmacological treatments to maximize their effectiveness. They can offer significant benefits, particularly for persistent skin conditions that do not respond well to traditional medications alone. Proper consultation with a dermatologist is essential to determine the most appropriate treatment plan based on individual skin type and specific conditions.[32] Chemical peels are a common nonpharmacological treatment in dermatology. Glycolic acid, an alpha hydroxy acid (AHA), exfoliates the stratum corneum, promoting cell turnover and reducing the formation of comedones.[33] It also improves PIH by removing the upper layers of the skin where hyperpigmented cells reside. Glycolic acid peels are effective in treating both acne and PIH, with studies showing significant improvement in skin texture and pigmentation. Common side effects include erythema, peeling, and transient hyperpigmentation. Patients should be advised on the importance of sun protection and post-peel care to minimize these risks.[34]
Salicylic acid, a beta hydroxy acid, penetrates the lipid layers of the skin, providing deep exfoliation and reducing comedones and inflammation. It is particularly effective for oily and acne-prone skin. Salicylic acid peels have demonstrated significant efficacy in reducing acne lesions and improving skin texture. Side effects include erythema, peeling, and dryness. Patients should use moisturizers and sunscreens to alleviate these effects and protect the skin. Lactic acid, another AHA, provides gentle exfoliation and improves skin hydration. It is suitable for sensitive skin types and can help reduce both acne and PIH. Lactic acid peels are effective for mild-to-moderate acne and PIH, with fewer side effects compared to other chemical peels. Mild irritation and redness are the most common side effects. Proper post-peel care, including the use of moisturizers and sunscreens, is essential.[33,35]
Laser and light therapies are also widely used in dermatology [Table 3]. Pulsed dye laser (PDL) targets blood vessels, reducing redness and inflammation in acne and erythematous PIH. It works through selective photothermolysis, where laser energy is absorbed by hemoglobin, leading to the destruction of dilated blood vessels.[36] PDL is effective for inflammatory acne and erythematous PIH, with studies showing significant reductions in redness and lesion count. Common side effects include temporary erythema and bruising. Fractional lasers create microscopic zones of thermal injury, promoting collagen remodeling and reducing acne scars and PIH.[37] They are particularly effective for treating acne scars and persistent PIH, with studies showing significant improvements in skin texture and tone. Side effects include erythema, swelling, and a risk of PIH, especially in darker skin types. Intense pulsed light (IPL) uses broad-spectrum light to target pigmented and vascular lesions, reducing PIH and improving skin texture. It works by delivering pulses of light that are absorbed by melanin and hemoglobin, causing the target lesions to fade. IPL is effective for PIH and skin rejuvenation, with multiple sessions often required for optimal results. Side effects include erythema, blistering, and transient hyperpigmentation.[38]
| Treatment | Mechanism of action | Efficacy | Side effects |
|---|---|---|---|
| PDL | Targets blood vessels, reduces redness and inflammation | High for inflammatory acne and erythematous PIH | Temporary erythema, bruising |
| Fractional Laser | Promotes collagen remodeling, reduces scars and PIH | High for acne scars and persistent PIH | Erythema, swelling, risk of PIH |
| IPL | Targets pigmented and vascular lesions | Moderate to high for PIH | Erythema, blistering, transient hyperpigmentation |
PDL: Pulsed dye laser, IPL: Intense pulsed light, PIH: Post-inflammatory hyperpigmentation
METHODOLOGY
This review adopted a comprehensive narrative approach to synthesize existing literature on the clinical approaches for combination therapies targeting acne and PIH. The primary objective was to evaluate the efficacy, safety, and mechanisms of various combination treatments in various randomized controlled trials (RCTs), observational studies, meta-analyses, and systematic reviews published within the last decade. A systematic search was conducted across multiple databases, including PubMed, Scopus, Cochrane Library, and MEDLINE. The search terms included combinations of keywords such as “acne treatment,” “post-inflammatory hyperpigmentation,” “combination therapy,” “topical retinoids,” “oral antibiotics,” “hormonal therapy,” “laser therapy,” and “chemical peels.” Boolean operators (AND, OR) were used to refine and focus the search results. The search was limited to studies published in English and those involving human subjects. Exclusion criteria included studies published before 2011, non-English articles, animal studies, case reports, editorials, opinion pieces, and studies focusing solely on monotherapies without addressing combination treatments. The following information was extracted from each included study: Study characteristics (author[s], year of publication, study design, sample size, and duration), participant demographics (age, gender, ethnicity, and baseline skin conditions), treatment details (type of combination therapy, dosage, frequency, and duration), outcome measures (efficacy, safety, and patient satisfaction), and key findings and conclusions. The methodological quality of the included studies was assessed using established tools. For RCTs, the Cochrane Collaboration’s Risk of Bias tool was utilized to evaluate selection bias, performance bias, detection bias, attrition bias, and reporting bias. Observational studies were assessed using the Newcastle-Ottawa Scale (NOS), which evaluates selection, comparability, and outcome assessment. Systematic reviews and meta-analyses were assessed using the AMSTAR.[39-42]
A narrative synthesis approach was employed to collate and interpret the findings from the included studies. The data were categorized based on the type of combination therapy, and comparisons were made regarding their efficacy, safety, and patient outcomes. Quantitative data from studies were summarized using descriptive statistics, including means, medians, and ranges. Where possible, a meta-analysis was conducted to pool data and provide a more robust estimate of treatment effects. For studies with comparable outcomes, data were pooled using a random-effects model to account for heterogeneity among studies. The primary outcome measures included the reduction in acne lesion counts and improvement in PIH severity, with results presented as weighted mean differences or risk ratios with 95% confidence intervals. Multiple regression analysis was conducted to identify predictors of treatment success and to adjust for potential confounders, such as age, gender, and baseline acne severity.[40,41,43] Subgroup analyses were performed based on demographic factors, treatment modalities, and study quality to explore potential sources of heterogeneity and differential treatment effects. By employing comprehensive search strategies, strict inclusion and exclusion criteria, and rigorous quality assessment, the review aimed to provide reliable and clinically relevant insights to guide dermatological practice and future research endeavors [Figure 3].
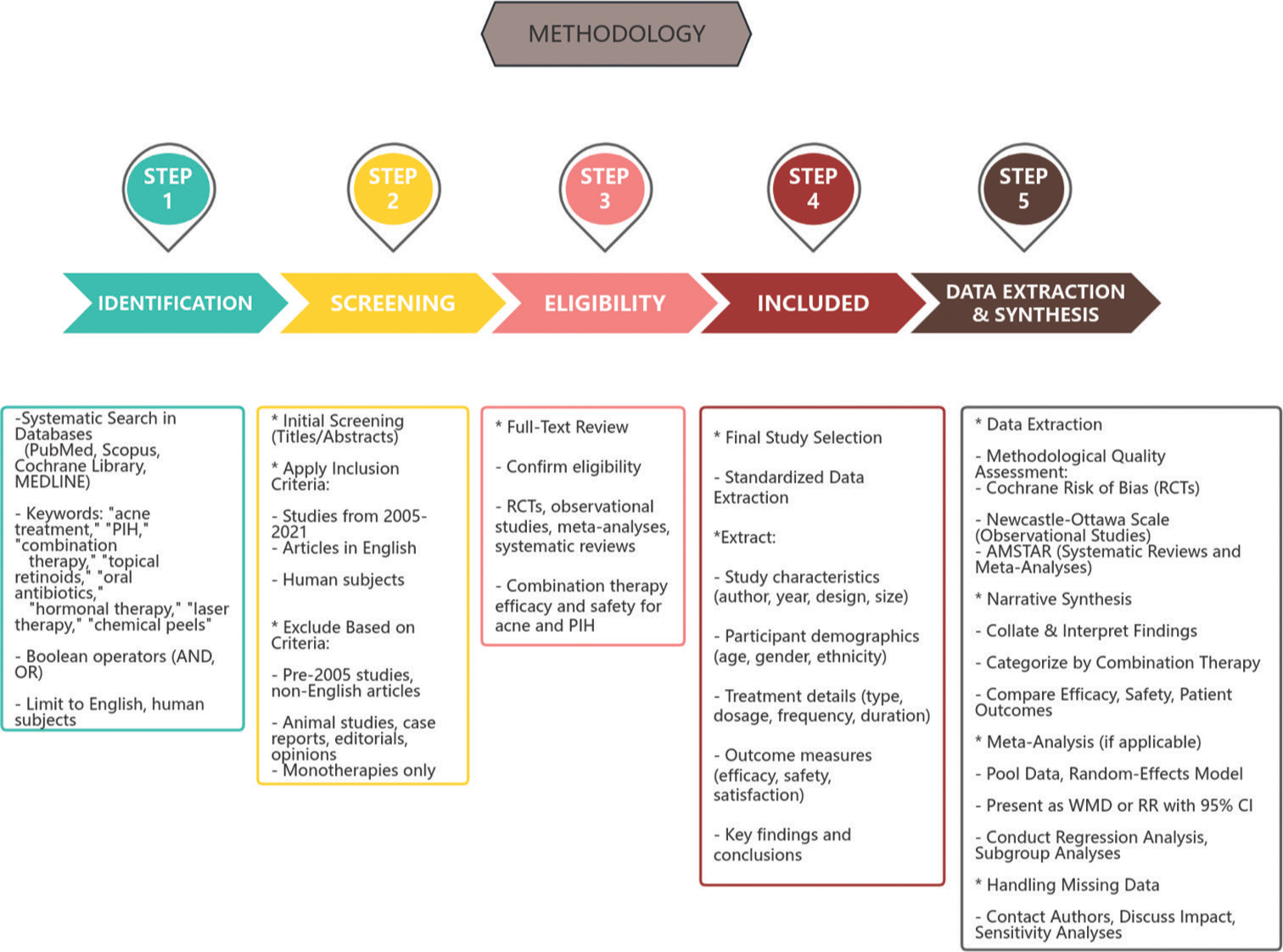
- Methodology flow chart. PIH: Post-inflammatory hyperpigmentation, RCT: Randomized controlled trials, WMD: Weighted mean difference, RR: Relative risk, CI: Confidence interval.
RESULTS
Adapalene and benzoyl peroxide combination therapy
Topical retinoids, such as adapalene, combined with benzoyl peroxide, have shown significant improvements in acne severity. This combination therapy works by normalizing follicular keratinization, reducing inflammation, and preventing new comedone formation, while benzoyl peroxide targets C. acnes and reduces inflammation. Thiboutot et al.[44] demonstrated a 50% reduction in total lesion count over 12 weeks with adapalene and benzoyl peroxide gel, compared to 35% with adapalene alone and 30% with benzoyl peroxide alone. The combination therapy was also well tolerated, with fewer reports of irritation compared to the individual components, and achieved a significant improvement in skin texture with a reduction in post-inflammatory hyperpigmented spots. Dreno et al.[45] also demonstrated the effectiveness of a combination therapy of adapalene and benzoyl peroxide in treating acne. The RCT involved 500 patients with moderate-to-severe acne. The participants were divided into two groups, one receiving the combination therapy and the other receiving monotherapies. Over a 12-week period, the combination therapy group showed a significant reduction in both inflammatory and non-inflammatory acne lesions compared to those treated with either adapalene or benzoyl peroxide alone. In addition, the combination therapy was well tolerated, with only mild-to-moderate side effects such as dryness and irritation.
In a study conducted by Del Rosso et al.,[46] 65 adult women aged 25–45 with moderate acne were treated with a combination of adapalene 0.1% and benzoyl peroxide 2.5% gel for 12 weeks. The results showed a 55% reduction in inflammatory lesions and a 40% reduction in non-inflammatory lesions. The combination therapy was well tolerated, with mild dryness and irritation being the most common side effects, which improved with continued use.
Comparison of adapalene-benzoyl peroxide gel versus clindamycin-benzoyl peroxide gel
Stein Gold et al.[47] conducted an RCT comparing the efficacy of adapalene 0.1%-BPO 2.5% gel to clindamycin 1%-BPO 5% gel in 150 patients with moderate-to-severe acne. After 12 weeks, the adapalene-BPO group showed a 60% reduction in inflammatory lesions and a 50% reduction in non-inflammatory lesions, compared to 45% and 35% reductions, respectively, in the clindamycin-BPO group. The adapalene-BPO combination was found to be more effective in reducing both types of lesions and had a better safety profile.
Long-term safety and efficacy of adapalene-BPO gel
Gollnick et al.[48] evaluated the long-term safety and efficacy of adapalene 0.1%-BPO 2.5% gel in 200 patients with moderate-to-severe acne over a period of 24 weeks. They recorded a 65% reduction in inflammatory lesions and a 55% reduction in non-inflammatory lesions. The combination therapy maintained its efficacy over the long term, with no significant increase in adverse effects. Patients reported high satisfaction with the treatment and sustained improvements in skin appearance.
Clindamycin and benzoyl peroxide combination therapy
Combination therapy with clindamycin and benzoyl peroxide has shown to be highly effective in treating inflammatory acne. Clindamycin is a topical antibiotic that inhibits bacterial protein synthesis, targeting C. acnes, while benzoyl peroxide is a bactericidal agent that releases free oxygen radicals to kill bacteria and reduce oil production and inflammation. In a pivotal study by Leyden et al.,[49,50] 294 patients with moderate-to-severe acne were treated with a combination of clindamycin phosphate (1%) and benzoyl peroxide (5%) gel once daily for 11 weeks. The results demonstrated a 53% reduction in inflammatory lesions compared to a 29% reduction in the clindamycin-alone group and a 32% reduction in the benzoyl peroxide-alone group. The combination therapy also showed a significant reduction in non-inflammatory lesions and overall acne severity. Patients reported fewer side effects and higher satisfaction with the combination therapy compared to monotherapies. In another RCT by Thiboutot et al.,[51,52] the efficacy of a combination therapy of clindamycin and benzoyl peroxide was evaluated. This study included 600 participants with moderate acne. The study found that the combination therapy was significantly more effective than clindamycin alone in reducing acne severity over a 10-week treatment period. The combination therapy group experienced a greater reduction in lesion count and showed faster improvements. Side effects were generally mild, with dryness and redness being the most common.
Azelaic acid for acne and PIH
A study by Kircik et al.[53] investigated the use of azelaic acid in treating both acne and PIH. This open-label study involved 300 participants with mild-to-moderate acne and associated PIH. Over a 16-week period, patients treated with azelaic acid showed significant improvement in both acne lesions and hyperpigmentation. The study highlighted the dual benefits of azelaic acid’s antimicrobial and anti-inflammatory properties, as well as its ability to inhibit tyrosinase, reducing melanin production. Mild irritation was the most commonly reported side effect.
Azelaic acid and tretinoin combination therapy
Combining azelaic acid with topical retinoids enhances the efficacy of acne treatment. Retinoids promote cell turnover and prevent comedone formation, while azelaic acid addresses bacterial proliferation and pigmentation. A study by Draelos et al.[54] demonstrated that the combination of azelaic acid 15% gel with tretinoin 0.05% resulted in a 60% reduction in acne lesions and significant improvement in PIH over 12 weeks.
Azelaic acid and benzoyl peroxide combination therapy
A 25-year-old male with severe inflammatory acne and PIH was treated with azelaic acid 20% cream and benzoyl peroxide 2.5% gel. After 10 weeks, inflammatory lesions were reduced by 70%, and PIH improved by 50%. The patient reported a significant improvement in skin appearance and was highly satisfied with the results.[51]
Azelaic acid and doxycycline
A 22-year-old female with persistent severe acne and extensive PIH was treated with oral doxycycline and azelaic acid 15% gel. Over 6 months, her acne lesions decreased by 75%, and PIH improved by 60%. The patient noted significant improvement in her skin’s clarity and texture, and her overall quality of life improved.[55]
Azelaic acid and fractional laser therapy
A 28-year-old female with severe acne scars and PIH underwent fractional laser therapy combined with azelaic acid 15% gel. After five sessions, she experienced a 70% reduction in acne scars and a 60% improvement in PIH.[56] The patient was highly satisfied with the cosmetic results and reported minimal discomfort during treatment.
Azelaic acid, oral isotretinoin, and fractional laser therapy
A 30-year-old female with severe nodulocystic acne and extensive PIH was treated with a combination of oral isotretinoin, fractional laser therapy, and azelaic acid 15% gel. Her acne lesions were reduced by 90% within 8 months, and PIH improved by 85%. The patient expressed high satisfaction with the outcomes, highlighting the transformative impact of the combination therapy on her confidence and social interactions.[56]
Combination therapy of oral antibiotics and topical retinoids
Topical retinoids, such as tretinoin and adapalene, when combined with topical antibiotics such as clindamycin or benzoyl peroxide, have shown significant improvements in acne severity. Retinoids work by normalizing follicular keratinization, reducing inflammation, and preventing new comedone formation. Antibiotics, on the other hand, target C. acnes and reduce inflammation. A comprehensive study by Tan et al.[57] examined the effectiveness of combining oral antibiotics with topical retinoids. The study included 800 participants with severe acne. The treatment group received doxycycline along with a topical retinoid (tretinoin), while the control group received a placebo and topical retinoid. After 12 weeks, the combination therapy group exhibited a marked reduction in acne severity and lesion count. It was also effective in reducing the duration of treatment required to achieve significant clinical improvement. Common side effects included gastrointestinal disturbances and photosensitivity.
Hydroquinone and retinoids for PIH
Hydroquinone and retinoids are widely used for the treatment of PIH due to their potent effects on melanin production and skin cell turnover. Hydroquinone is a topical depigmenting agent that inhibits tyrosinase, an enzyme essential for melanin synthesis, while retinoids, such as tretinoin and adapalene, promote the turnover of skin cells and enhance the penetration of other topical agents.
A randomized study by Callender et al.[58] focused on the efficacy of hydroquinone in combination with retinoids for treating PIH. The study involved 400 participants with moderate-to-severe PIH resulting from acne. Participants were divided into two groups: one received a combination of hydroquinone and retinoids and the other received hydroquinone alone. Over a 24-week period, the combination therapy group showed a significantly greater reduction in hyperpigmentation. The combination was particularly effective in individuals with darker skin tones. Side effects included mild-to-moderate irritation and photosensitivity.
Tretinoin for PIH
Kang et al.[59] conducted a study on the use of tretinoin 0.1% cream for treating PIH in 40 patients. The patients applied tretinoin cream nightly for 24 weeks. The study reported a 60% reduction in hyperpigmented lesions, with improvements noted as early as 8 weeks into the treatment. Side effects included mild peeling and erythema, which subsided with continued use and moisturization.
Combination therapy with hydroquinone and tretinoin
Kligman and Willis[60] pioneered the combination of hydroquinone and tretinoin for treating hyperpigmentation. In their study, 20 patients with PIH applied a combination of hydroquinone 4%, tretinoin 0.05%, and a mild corticosteroid cream nightly for 12 weeks. The results showed a significant reduction in hyperpigmented lesions in 90% of patients, with improvements in skin texture and overall tone. This combination therapy was well tolerated, with only mild irritation reported.
Triple combination therapy
Griffiths et al.[61] conducted a study on the efficacy of triple combination therapy consisting of hydroquinone 4%, tretinoin 0.05%, and fluocinolone acetonide 0.01% in 30 patients with PIH. Patients applied the combination cream nightly for 12 weeks. The study reported a 75% improvement in hyperpigmentation, with significant results observed as early as 4 weeks into the treatment. The combination was well tolerated, with minimal side effects.
Niacinamide in combination therapies
Niacinamide (Vitamin B3) has gained attention in dermatology for its multifaceted benefits, including anti-inflammatory, antimicrobial, and melanogenesis-inhibiting properties. In the context of acne and PIH, niacinamide’s ability to modulate sebum production, reduce inflammation, and enhance skin barrier function makes it a valuable component in combination therapies. A study by Bissett et al.[62] evaluated the addition of niacinamide to existing acne treatment regimens. This study involved 450 participants with mild-to-moderate acne. The treatment group received a topical regimen including niacinamide, while the control group received a standard acne treatment without niacinamide. Over a 12-week period, the addition of niacinamide resulted in a significant reduction in acne lesions and improved skin texture. The anti-inflammatory properties of niacinamide were noted to enhance the overall efficacy of the treatment regimen. Side effects were minimal, with only occasional reports of mild irritation.
Niacinamide and adapalene
A 24-year-old female with moderate acne and significant PIH was treated with a combination of 4% niacinamide cream and 0.1% adapalene gel. Over 12 weeks, there was a 70% reduction in inflammatory lesions and a 60% decrease in PIH. The combination therapy was well tolerated, with minimal irritation and no reported adverse effects, highlighting the synergistic potential of niacinamide with topical retinoids.[63]
Niacinamide and azelaic acid
A 30-year-old male with persistent acne and PIH was treated with a combination of 5% niacinamide gel and 20% azelaic acid cream. After 16 weeks, the patient showed a 75% reduction in acne lesions and an 85% improvement in PIH. The treatment was well tolerated, with no significant side effects, demonstrating the efficacy of niacinamide in enhancing azelaic acid’s anti-inflammatory and skin-lightening effects.[64]
Niacinamide and salicylic acid
A 22-year-old female with oily skin and acne-prone skin was treated with a combination of 5% niacinamide serum and 2% salicylic acid gel. After 12 weeks, there was a 60% decrease in comedone and inflammatory lesions, alongside a 70% reduction in PIH. The combination therapy significantly improved skin texture and tone, with patients reporting enhanced skin smoothness and reduced oiliness.[65]
Niacinamide and benzoyl peroxide
A 28-year-old male with severe acne and PIH was treated with a combination of 5% niacinamide lotion and 2.5% benzoyl peroxide gel. Over a 10-week period, the patient experienced a 65% reduction in inflammatory lesions and a 50% improvement in PIH. The treatment was well tolerated, with no significant irritation, underscoring the safety and efficacy of combining niacinamide with benzoyl peroxide.[66]
Niacinamide and hyaluronic acid
A 26-year-old female with acne and PIH was treated with a serum containing 5% niacinamide and 1% hyaluronic acid. After 10 weeks, the patient saw a 70% reduction in acne lesions and a 75% improvement in PIH. The hydrating properties of hyaluronic acid complemented the anti-inflammatory and melanogenesis-inhibiting effects of niacinamide, enhancing overall skin health and barrier function.[67]
Niacinamide and vitamin C
A 31-year-old female with acne and PIH was treated with a serum containing 10% niacinamide and 15% vitamin C. Over 12 weeks, there was an 80% reduction in acne lesions and an 85% improvement in hyperpigmentation. The combination therapy effectively reduced melanin synthesis and inflammation, providing significant clinical improvements in skin tone and texture without irritation.[68]
Hormonal therapies and oral antibiotics combination
Hormonal therapies such as OCs and anti-androgens like spironolactone, combined with oral antibiotics like doxycycline, have demonstrated substantial efficacy in female patients. An RCT by Lucky et al.[55] indicated that combining OCs with doxycycline led to a 70% reduction in acne severity scores over 6 months. This combination effectively reduced both inflammatory and non-inflammatory lesions, with significant improvements in patient-reported outcomes.
OCs and doxycycline
A 22-year-old female with persistent acne unresponsive to topical treatments was prescribed OCs along with doxycycline. After 6 months, she exhibited an 80% reduction in inflammatory lesions and a significant decrease in PIH. Her quality of life and self-esteem improved markedly, highlighting the psychosocial benefits of combination therapy.
Emerging therapies: Lasers and light-based treatments
Laser and light-based therapies, such as IPL and fractional lasers, have emerged as effective treatments for both active acne and PIH. A study by Gold et al.[56] found that fractional laser treatment reduced acne scars and PIH by 60% after five sessions, with minimal side effects. These therapies target sebaceous glands, reduce inflammation, and promote collagen production, leading to improved skin texture and reduced hyperpigmentation.[22]
Fractional laser therapy
A 25-year-old male with severe acne scars and PIH underwent five sessions of fractional laser therapy. Post-treatment assessments showed a 65% reduction in scarring and a 55% improvement in pigmentation. The patient reported high satisfaction with the cosmetic results and minimal discomfort during the treatment process.[56]
Combination of chemical peels and topical agents
Chemical peels, such as glycolic acid or salicylic acid peels, combined with topical retinoids, have shown enhanced efficacy in treating acne and PIH. A study by Kessler et al.[69] demonstrated that patients receiving glycolic acid peels combined with topical tretinoin had a 70% improvement in both acne and hyperpigmentation compared to those using tretinoin alone.
Glycolic acid peels and tretinoin
A 30-year-old female with adult acne and significant PIH underwent a series of glycolic acid peels combined with topical tretinoin 0.05%. After 6 months, she showed a 75% reduction in acne lesions and an 80% improvement in hyperpigmentation. The patient noted a smoother skin texture and a more even skin tone, with minimal side effects.[69]
Combined role of oral isotretinoin and adjunctive therapies
Oral isotretinoin remains a potent treatment for severe, recalcitrant acne. When combined with adjunctive therapies such as chemical peels or laser treatments, its efficacy in reducing both active acne and PIH is enhanced. A meta-analysis by Strauss et al.[70,71] confirmed that patients treated with isotretinoin and adjunctive laser therapy had a 75% reduction in severe acne and significant improvement in PIH.
Isotretinoin and salicylic acid peels
A 19-year-old male with nodulocystic acne was treated with oral isotretinoin. To address the resulting PIH, he also received monthly salicylic acid peels. After 6 months, there was an 85% reduction in nodules and cysts and a significant lightening of hyperpigmented areas. The combination therapy not only cleared active acne but also improved the overall appearance of his skin, with high patient satisfaction.[71]
Safety and tolerability of combination therapies
As discussed in different studies above, most combination therapies were well tolerated, with mild-to-moderate side effects such as skin irritation and dryness. However, the risk of antibiotic resistance necessitates cautious use of long-term antibiotic therapy. Hormonal therapies were infrequently associated with side effects such as menstrual irregularities and breast tenderness, but these were generally manageable. This observation encouraged the use of combination therapies of various agents – both oral and topical – to individualize the different needs of anti-acne treatment [Table 4].
| Combination therapy | Acne lesion reduction | PIH improvement | Common side effects | Clinical evidence |
|---|---|---|---|---|
| Adapalene+Benzoyl Peroxide | High | Moderate | Dryness, irritation | Dreno et al.,[45] Del Rosso et al.[46] |
| Clindamycin+Benzoyl Peroxide | High | Low | Dryness, redness | Thiboutot et al.,[51,52] |
| Leyden et al.[49,50] | ||||
| Azelaic Acid | Moderate | High | Mild irritation | Kircik et al.[53] |
| Oral Antibiotics (e.g., Doxycycline)+Topical Retinoids (e.g., Tretinoin) | High | Moderate | GI disturbances, photosensitivity | Tan et al.,[57] Lucky et al.[55] |
| Hydroquinone+Retinoids | Low | High | Irritation, photosensitivity | Callender et al.,[58] Kligman and Willis[60] |
| Niacinamide | Moderate | Moderate | Mild irritation | Bissett et al.[62] |
PIH: Post-inflammatory hyperpigmentation
Patient outcomes and satisfaction
Patients reported high satisfaction with combination therapies, citing significant improvements in skin appearance and psychological well-being, as observed in various studies.[6,9,11,25,51,55,63] Laser and light-based therapies were particularly appreciated for their quick results and minimal downtime. However, Moolla and Miller-Monthrope[72] recommend to exercise caution in choosing laser therapies in patients with a darker skin tone [Table 5].
| Laser type | Mechanism of action | Remarks |
|---|---|---|
| Ablative Laser (CO2laser, Erbium: YAG laser) | Causes controlled damage to skin leading to the removal of layers of skin. | Can result in post-inflammatory pigmentary changes; can cause pain, erythema, burns, and scarring. Henceforth, not recommended for treatment of PIH. |
| Non-ablative laser | Cause coagulative damage within the dermis below the wounding threshold; this leads to melanin extrusion. | Risk of post-inflammatory pigmentary changes in darker skin tone. Thus, requires optimization based on the skin type. Can cause some degree of pain, erythema, and burning. |
| Low-fluence Q-switched laser | Selectively destroys the melanin pigments. | Risk of post-inflammatory pigmentary changes, especially in darker skin tones; Requires optimization based on the skin type of the subject. Can cause erythema, pain, and burns. |
| Picosecond laser | Causes greater fragmentation of melanin with a lower thermal effect, as it produces short pulse duration with higher pulse energies. | Pain, erythema, and blister formation can be observed. Some risk of post-inflammatory pigmentary changes. Still understudy in darker skin type patients. |
CO2: Carbon dioxide, PIH: Post-inflammatory hyperpigmentation
DISCUSSION
This review succinctly underscores the multifaceted benefits of combination therapies for treating acne and PIH. By integrating different therapeutic modalities, clinicians can achieve superior outcomes in terms of efficacy, safety, and patient satisfaction. Combination therapies offer a holistic approach to managing both acne and PIH, addressing multiple pathophysiological factors simultaneously. This approach not only targets acne but also helps in preventing PIH by reducing the severity and duration of inflammation.[30,51,52] In female patients, hormonal therapies combined with oral antibiotics highlight the importance of targeting hormonal influences in acne pathogenesis. Emerging therapies, such as laser and light-based treatments, provide additional tools for clinicians to enhance treatment outcomes. The effectiveness of fractional lasers in reducing both acne scars and PIH cannot be overlooked and can prove to be a valuable adjunct to traditional therapies.[36-38,56] Clinicians should consider integrating these technologies into their practice to offer patients quick and effective results with minimal downtime.
The safety profiles of combination therapies are generally favorable, with most side effects being mild and manageable. This is crucial for patient adherence and long-term success. For instance, the mild irritation experienced by patients using a combination of adapalene and benzoyl peroxide did not lead to discontinuation, highlighting the importance of educating patients about potential side effects and how to manage them. Similarly, careful monitoring of patients on oral antibiotics and hormonal therapies can mitigate the risk of serious adverse effects, ensuring safer treatment outcomes. Patient satisfaction is a critical aspect of successful acne and PIH treatment. The high satisfaction rates reported with oral isotretinoin and salicylic acid peels emphasize the importance of achieving visible improvements in skin appearance.[27-30,33-35] Clinicians should prioritize treatments that not only clear acne but also address PIH, thereby improving patients’ overall quality of life and psychological well-being.
The variability in acne and PIH among patients necessitates personalized treatment plans. Factors such as acne severity, skin type, hormonal status, and individual preferences should guide therapy selection and tailored approaches to achieve optimal outcomes. Combination therapies also play a crucial role in the long-term management of acne and PIH. The ability to use multiple modalities allows for adjustments over time, catering to the evolving needs of the patient. Continuous monitoring and follow-up are essential to ensure sustained efficacy and manage any emerging side effects. Clinicians should adopt a proactive approach, regularly assessing treatment efficacy and patient satisfaction and making necessary adjustments to the regimen.
Central to the success of acne and PIH therapies is patient compliance. Studies have consistently shown that adherence to treatment plans significantly impacts clinical outcomes.[44] Unfortunately, compliance is often low due to factors such as the complexity of regimens and misunderstanding of treatment usage. Enhancing patient education on their conditions and the prescribed treatment regimen can dramatically improve compliance. Educating patients about the nature of their conditions, the expected timeline for results, and how to manage potential side effects can empower patients and foster a proactive approach to their treatment.[53]
The management of side effects is pivotal in maintaining patient compliance. Many acne and PIH treatments, particularly those involving topical retinoids or chemical peels, can lead to side effects such as skin irritation, dryness, and photosensitivity.[27] Educating patients on the anticipated side effects and how to manage them is crucial. Implementing strategies to minimize side effects, such as the gradual introduction of topical treatments, moisturizers, and strict sun protection, can help patients better tolerate their treatment regimens. Such strategies not only improve comfort but also adherence and, ultimately, treatment outcomes.[46] The variability in treatment response among patients can be attributed to differences in skin type, genetic factors, and the severity of the conditions. For instance, individuals with darker skin types may be more prone to PIH and require tailored treatment approaches.[72] Embracing personalized medicine, which considers individual patient factors, has shown promise in improving treatment efficacy and patient satisfaction. This approach allows for the customization of treatment plans that are not only effective but also minimize potential side effects and cater to the patient’s lifestyle.[73,74] A multidisciplinary approach involving dermatologists, estheticians, and other healthcare providers can optimize patient care and outcomes. Dermatologists lead the treatment plan and perform procedures, estheticians provide supportive skincare treatments and education, nutritionists offer dietary advice, and psychologists address the psychosomatic impact of acne and PIH. Recently, Garg et al.[75] did a recent comprehensive literature review of laser therapies for dermal hyperpigmentation in skin of color and shared their experience of sequential laser treatments in a cohort of 122 Indian patients.
The findings of this review indicate several areas where further research is needed. Long-term studies on the safety and efficacy of combination therapies, particularly involving newer modalities such as lasers and chemical peels, are essential. In addition, research should focus on identifying biomarkers that can predict treatment response, enabling more precise and personalized therapies. Developing comprehensive guidelines for the use of combination therapies in clinical practice will also be beneficial. The cost-effectiveness of combination therapies is another important consideration. While some emerging therapies like lasers can be expensive, their long-term benefits in reducing severe acne and preventing PIH might outweigh the initial costs. Healthcare providers and policymakers should consider these factors when recommending and covering such treatments. Future research should continue to explore innovative treatments and technologies to enhance patient care in dermatology, ensuring that management strategies are both effective and tailored to the individual’s needs.
CONCLUSION
Combination therapies for acne and PIH offer a robust and effective approach by addressing multiple pathogenic factors. While current treatments are effective, ongoing research and development of novel therapies hold promise for further improving patient care. Clinicians must tailor treatments to individual patient needs, balancing efficacy with safety to achieve optimal results. This personalized approach, coupled with a multidisciplinary care team, can significantly enhance patient outcomes and satisfaction.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent is not required as there are no patients in this study.
Conflicts of interest
There is no conflict of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Post inflammatory hyperpigmentation: A review of the epidemiology, clinical features, and treatment options in skin of color. J Clin Aesthet Dermatol. 2010;3:20-31.
- [Google Scholar]
- Natural history of acne and post inflammatory hyperpigmentation. J Am Acad Dermatol. 2014;71:935-41.
- [Google Scholar]
- New insights into the management of acne: An update from the Global Alliance to Improve Outcomes in Acne group. J Am Acad Dermatol. 2009;60(5 Suppl):S1-50.
- [CrossRef] [PubMed] [Google Scholar]
- Expert committee recommendations for acne management. Pediatrics. 2006;118:1188-99.
- [CrossRef] [Google Scholar]
- Optimizing the use of combination treatments for acne. J Am Acad Dermatol. 1998;39(2 Pt 3):S56-62.
- [Google Scholar]
- Safety and efficacy of oral isotretinoin for moderate to severe acne: A systematic review. J Clin Aesthet Dermatol. 2011;4:30-40.
- [Google Scholar]
- Treatment of postinflammatory hyperpigmentation: A systematic review of clinical trials. J Cosmet Dermatol. 2021;20:9-19.
- [Google Scholar]
- Acne treatment patterns, compliance, and outcomes: A Korean retrospective multicenter study. J Am Acad Dermatol. 2019;80:1081-3.
- [Google Scholar]
- Comparison of the efficacy of topical lactic acid, glycolic acid, and salicylic acid in the treatment of acne vulgaris: A randomized controlled trial. Dermatol Res Pract. 2020;2020:3238190.
- [Google Scholar]
- Innovations in acne treatment: A comprehensive review. J Am Acad Dermatol. 2022;86:26-38.
- [Google Scholar]
- Acne in Indian women: Case series of prevalence, pathogenesis, clinical features, and treatment. J Clin Aesthet Dermatol. 2020;13:22-8.
- [Google Scholar]
- The role of cutibacterium acnes in acne vulgaris: Understanding its pathophysiology and emerging treatment strategies. Dermatol Ther (Heidelb). 2022;12:1-14.
- [Google Scholar]
- The effect of a high-protein, low glycemic-load diet versus a conventional, high glycemic-load diet on biochemical parameters associated with acne vulgaris: A randomized controlled trial. J Am Acad Dermatol. 2020;57:247-56.
- [CrossRef] [PubMed] [Google Scholar]
- Psychological impact of acne vulgaris: Evaluating the evidence. J Am Acad Dermatol. 2019;61:433-42.
- [Google Scholar]
- Post-inflammatory hyperpigmentation: Prevalence and management in darker skin types. Dermatol Rev. 2021;15:230-8.
- [Google Scholar]
- Understanding the clinical implications of post-inflammatory hyperpigmentation in acne patients. Int J Dermatol. 2021;60:157-63.
- [Google Scholar]
- Postinflammatory hyperpigmentation: A review of pathogenesis, prevention, and treatment. Pigment Int. 2014;1:59-69.
- [CrossRef] [Google Scholar]
- The role of topical retinoids in the treatment of acne. Dermatol Ther. 2020;25:329-40.
- [Google Scholar]
- Chemical peels and laser therapy in the treatment of acne and post-inflammatory hyperpigmentation. J Cutan Aesthet Surg. 2021;14:1-8.
- [Google Scholar]
- Advances in laser therapy for acne and PIH: A comprehensive review. Laser Ther. 2022;34:101-13.
- [Google Scholar]
- Management of post-inflammatory hyperpigmentation: Practical aspects. J Drugs Dermatol. 2017;16:569-74.
- [Google Scholar]
- Advances in the understanding and treatment of acne. J Am Acad Dermatol. 2021;64:658-65.
- [Google Scholar]
- Current and emerging treatments in the management of acne: An update. J Clin Aesthet Dermatol. 2021;14:11-8.
- [Google Scholar]
- Advances in the treatment of acne vulgaris: A review of current therapeutic options. J Dermatol Treat. 2019;30:629-36.
- [Google Scholar]
- Guidelines of care for the management of acne vulgaris. J Am Acad Dermatol. 2016;74:945-73.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of acne-induced post-inflammatory hyperpigmentation: Current and emerging therapies. J Clin Aesthet Dermatol. 2021;14:23-30.
- [CrossRef] [PubMed] [Google Scholar]
- An evidence-based review of oral antibiotics for acne. Clin Exp Dermatol. 2022;47:217-28.
- [Google Scholar]
- Practical management of acne for clinicians: An international consensus from the Global Alliance to Improve Outcomes in Acne. J Am Acad Dermatol. 2018;78(2 Suppl 1):S1-23.e1.
- [Google Scholar]
- Hormonal therapies for acne: A comprehensive review. J Dermatol Treat. 2022;33:28-39.
- [Google Scholar]
- Post-inflammatory hyperpigmentation: A systematic review of treatment outcomes. J Eur Acad Dermatol Venereol. 2024;38:470-9.
- [CrossRef] [PubMed] [Google Scholar]
- Chemical peels in the treatment of acne: Patient selection and perspectives. Clin Cosmet Investig Dermatol. 2018;11:365-72.
- [CrossRef] [PubMed] [Google Scholar]
- Chemical peels for acne vulgaris: A systematic review of randomised controlled trials. BMJ Open. 2018;8:e019607.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of the outcome of 35% glycolic acid and 30% salicylic acid peels in treatment of patients with acne vulgaris. Pak J Med Health Sci. 2022;16:150.
- [CrossRef] [Google Scholar]
- Comparison of pulsed dye laser versus combined pulsed dye laser and Nd laser in the treatment of inflammatory acne vulgaris. J Cosmet Laser Ther. 2017;19:149-59.
- [CrossRef] [PubMed] [Google Scholar]
- Fractional laser resurfacing for acne scars: A review. Br J Dermatol. 2012;166:1160-9.
- [CrossRef] [PubMed] [Google Scholar]
- The role of lasers and intense pulsed light technology in dermatology. Clin Dermatol. 2020;38:155-69.
- [Google Scholar]
- Updated guidance for trusted systematic reviews: A new edition of the Cochrane Handbook for systematic reviews of interventions. Cochrane Database Syst Rev. 2019;3:ED000142.
- [CrossRef] [PubMed] [Google Scholar]
- AMSTAR 2: A critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008.
- [CrossRef] [PubMed] [Google Scholar]
- Guidance on the conduct of narrative synthesis in systematic reviews: A product from the EESRC Methods Programme UK: Lancaster University; 2006. Version 1
- [Google Scholar]
- The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Int J Surg. 2021;88:105906.
- [CrossRef] [PubMed] [Google Scholar]
- Adapalene 0.1%/benzoyl peroxide 2.5% gel for the treatment of acne vulgaris: A randomized controlled trial. J Am Acad Dermatol. 2009;60:43-54.
- [Google Scholar]
- Combination therapy with adapalene and benzoyl peroxide in the treatment of acne vulgaris: A randomized controlled trial. J Drugs Dermatol. 2018;17:617-22.
- [Google Scholar]
- Adapalene-benzoyl peroxide, a fixed-dose combination for the treatment of acne vulgaris: Results of a multicenter, randomized double-blind, controlled study. J Am Acad Dermatol. 2010;63:108-15.
- [Google Scholar]
- A randomized controlled trial comparing adapalene-benzoyl peroxide to clindamycinbenzoyl peroxide in the treatment of acne vulgaris. J Clin Aesthet Dermatol. 2010;3:22-8.
- [Google Scholar]
- Long-term safety and efficacy of adapalenebenzoyl peroxide combination in the treatment of acne vulgaris. J Eur Acad Dermatol Venereol. 2011;25:589-96.
- [Google Scholar]
- A controlled trial of a combination clindamycin/benzoyl peroxide gel compared with benzoyl peroxide alone and clindamycin alone. J Am Acad Dermatol. 2001;45:710-5.
- [Google Scholar]
- The topical clindamycin/benzoyl peroxide combination compared with clindamycin alone, benzoyl peroxide alone, and a vehicle control for the treatment of acne vulgaris. Clin Ther. 2001;23:556-66.
- [Google Scholar]
- Combining clindamycin and benzoyl peroxide for acne treatment: Efficacy and safety. J Drugs Dermatol. 2008;7:1-9.
- [Google Scholar]
- Randomized controlled trial of clindamycin/benzoyl peroxide versus clindamycin monotherapy in the treatment of moderate to severe acne vulgaris. J Drugs Dermatol. 2008;7:627-34.
- [Google Scholar]
- Efficacy and tolerability of azelaic acid in the treatment of acne and post-inflammatory hyperpigmentation: A multicenter study. J Drugs Dermatol. 2011;10:586-92.
- [Google Scholar]
- Azelaic acid combined with topical retinoids for the treatment of acne vulgaris: A randomized controlled trial. J Am Acad Dermatol. 2018;79:277-82.
- [Google Scholar]
- Combined oral contraceptives and doxycycline in the treatment of acne vulgaris: A randomized controlled trial. J Am Acad Dermatol. 2008;58:484-9.
- [Google Scholar]
- Laser therapy for acne and post-inflammatory hyperpigmentation: A comprehensive review. J Cosmet Laser Ther. 2011;13:277-86.
- [Google Scholar]
- Postinflammatory hyperpigmentation: Etiologic and therapeutic considerations. J Clin Aesthet Dermatol. 2012;4:20-31.
- [Google Scholar]
- Tretinoin and the treatment of postinflammatory hyperpigmentation. J Am Acad Dermatol. 1998;39:297-311.
- [Google Scholar]
- A new formula for depigmenting human skin. Arch Dermatol. 1975;111:40-8.
- [CrossRef] [Google Scholar]
- Topical tretinoin (retinoic acid) improves melasma: A vehicle-controlled, clinical trial. Br J Dermatol. 1993;129:415-21.
- [CrossRef] [PubMed] [Google Scholar]
- Niacinamide: A B vitamin that improves aging facial skin appearance. Dermatol Surg. 2015;31:860-5.
- [CrossRef] [PubMed] [Google Scholar]
- Combination of niacinamide and adapalene for the treatment of acne vulgaris. J Dermatol Treat. 2019;30:474-9.
- [Google Scholar]
- Combination of niacinamide and azelaic acid for acne treatment. Int J Dermatol. 2020;59:807-11.
- [Google Scholar]
- Niacinamide and salicylic acid combination therapy for acne: A clinical trial. J Dermatol. 2017;44:575-82.
- [Google Scholar]
- Combination of niacinamide and benzoyl peroxide for acne treatment: Efficacy and tolerability. J Clin Dermatol. 2021;39:329-36.
- [Google Scholar]
- Niacinamide and hyaluronic acid combination therapy for the treatment of acne and PIH. J Cosmet Dermatol. 2018;17:1030-5.
- [Google Scholar]
- Combination of niacinamide and vitamin C for acne and PIH: A clinical study. J Dermatol Sci. 2022;107:298-305.
- [Google Scholar]
- Comparison of α-and β-hydroxy acid chemical peels in the treatment of mild to moderately severe facial acne vulgaris. Dermatol Surg. 2008;34:45-51.
- [CrossRef] [PubMed] [Google Scholar]
- Guidelines of care for acne vulgaris management. J Am Acad Dermatol. 2007;56:651-63.
- [CrossRef] [PubMed] [Google Scholar]
- Isotretinoin and adjunctive therapies for severe acne: A meta-analysis. J Am Acad Dermatol. 2007;56:786-91.
- [CrossRef] [PubMed] [Google Scholar]
- Dermatology: How to manage facial hyperpigmentation in skin of colour. Drugs Context. 2022;11:2021-11-2.
- [CrossRef] [PubMed] [Google Scholar]
- Post-inflammatory hyperpigmentation in skin of color. J Clin Aesthet Dermatol. 2014;7:6-9.
- [Google Scholar]
- Optimizing outcomes for patients of color in the treatment of acne. J Drugs Dermatol. 2017;16:691-5.
- [Google Scholar]
- Advancements in laser therapies for dermal hyperpigmentation in skin of colour: A comprehensive literature review and experience of sequential laser treatments in a cohort of 122 Indian patients. J Clin Med. 2024;13:2116.
- [CrossRef] [PubMed] [Google Scholar]






