Translate this page into:
Tattoo regret

*Corresponding author: Anuja Rao, Department of Dermatology and STD, Maulana Azad Medical College, New Delhi, India. anujarao12@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Rao A, Yadav P. Tattoo regret. CosmoDerma. 2024;4:112. doi: 10.25259/CSDM_70_2024
Abstract
Tattooing has been in practice since millenniums across the globe for various purposes such as art and beautification. Recently, a new perspective has become popular, particularly among youngsters as a fashion statement, an improvement of body image and as an expression of affection toward their loved ones. Various side effects such as infections, allergic contact dermatitis, scarring and granuloma formation, and inflammatory reactions have also been associated with tattooing. Tattoo regret is also on the rise with the increase in tattooing. The most common motivation for the removal of a tattoo is the enhancement of self-esteem. Other reasons for removal include eradication of a socially discrediting lesion, domestic pressure, and improvement of employment prospects.
Keywords
Tattoos
Regret
Koebner phenomenon
Tattooing has become a global trend and is quite popular worldwide among adolescents and young adults. A tattoo is the insertion of an exogenous pigment into the skin or mucous membranes. The word tattoo has two major derivations: The first is from the Polynesian word “ta,” which means “striking something,” and the second Tahitian word “tatau,” which means “to mark something.”[1] Evidence of tattooing has been found worldwide since the olden days.[2] It began in Egypt as early as 4000 BCE. Then, the practice spreads east into South Asia and west to the British Isles and Scotland. The Iberians in the British Isles, the Picts in Scotland, the Gauls in Western Europe, and the Teutons in Germany all practiced tattooing, and the Romans were known to use tattooing to mark convicts and slaves.[2] By 787 AD, tattooing was prevalent enough to warrant an official ban by Pope Hadrian I at the Second Ecumenical Council of Nicaea.[1] Tahiti in 1769 and Hawaii in 1778, Cook encountered heavily tattooed populations who deposited dye into the skin by tapping sharpened instruments.[3] The first tattooed people were displayed in the United States at the Centennial Exhibition in Philadelphia, Pennsylvania, in 1876.[1] Later, at the 1901 World’s Fair in Buffalo, New York, the first full “freak show” emerged, and tattooed “natives” were displayed.[4] The first professional tattooist in the United States, Martin Hildebrandt opened his shop in New York City, New York, in 1891. In 1891, Samuel O’Reilly, an American tattoo artist patented the first electric tattooing machine. The popularity of tattoos has surged across cultures, geographical areas, social classes, and levels of education, more so in recent years – probably due to digital media and the commercialization of culture.
The prevalence of tattooing in these age groups varies by country and setting, ranging from 1% to 24%.[3] In India, there is mushrooming of tattoo parlors in almost all of the major cities. The prevalence of tattooing is about 10–29% worldwide.[5] In Western society, tattooing has become one of the mainstream activities among adolescents and young adults. Tattooing has been classified as accidental or deliberate, permanent or temporary, professional or amateur, cosmetic, and decorative or medical. During tattooing with a tattoo machine, a large amount of ink is injected, about 0.4– 14.36 mg of pigment. The inks used for tattooing contain a multi-component mixture of chemical compounds, with the coloring components (pigments and colorants) being the main components responsible for the visual effect and color. The inks contain heavy metals such as chromium (green and blue colorants), cobalt (e.g., yellow and blue colorants), and lead, antimony, arsenic, beryllium as well as nickel and mercury (red colorant) often classified by the International Agency for Research on Cancer (IARC) as carcinogenic or potentially carcinogenic compounds. In addition, the presence of aromatic amines, phthalates, polycyclic aromatic hydrocarbons, and nanoparticles has been confirmed.[4]
Reasons for tattooing differ among populations, societies, age groups, and time periods. In the olden days, tattoos were used for therapeutic purposes and used as a system of knowledge transmission.[6,7] However, religions such as Christianity and Judaism have taken an unfavorable view of tattoos, they continue to play a deep religious and cultural role in some societies as devotion, power, and magical abilities also provide identity and guidance in the afterlife.[8] In recent years, motivations include personal symbolism, expression of shared values within a subculture, quest for individuality, enhancing attractiveness, rebellion, fashion, using the body as a canvas for art, peer pressure, and impulsive tattooing under the influence of alcohol and drugs.[7-9] The motivation also varies with social circumstances and education.[7] Less than 10% of tattoos are now initiated under the influence of alcohol or drugs, and in this group, those with only a high-school education are disproportionately represented.[7,9] There is a rich cultural heritage of tattooing in the tribes of North-East India. Tattooing was more of a social issue than a personal choice in the early days. Even in India, the tattoo culture has shifted significantly among adolescents and young adults. In recent years, tattooing has increased in popularity among adolescents as a fashion statement or improvement of body image.[10] This could probably be attributed to urbanization, digital media celebrities, sports icons, and peers.
Tattoos are not without risk after all. Patients are at risk for developing infections, allergic contact dermatitis, pseudolymphoma, and inflammatory reactions. Most people who have undergone tattoo making are unaware of the health-related risks associated with it. It was reported in a study from Manipur that 87% of subjects had inadequate knowledge of the health risks associated with it.[3]
However, there has been a remarkable increase in the number of patients seeking removal of tattoos for various reasons. The three major reasons mentioned in Western studies for laser tattoo removal were “Never been pleased with tattoo,” “Embarrassment or shame,” and “Professional reasons.”[11] The reasons for laser tattoo removal in another study were improvement of self-esteem followed by social reasons, family pressure, improving potential for employment, and a change of partner.[11,12] In Indian studies, the major reason for tattoo removal was to be eligible for armed force jobs, followed by regret, elder or school pressure, and personal and unsightly appearance such as hypertrophic scarring in the tattoo.
Laser tattoo removal is the most common method used to remove or lighten tattoos. The laser light energy shatters the tattoo ink into small particles, which the body’s immune system clears over time. The type of laser used to remove a tattoo depends on the tattoo’s colors. Because different colors of ink absorb different wavelengths of light, multi-colored tattoos may require the use of multiple lasers. Colors such as green, red, and yellow are the hardest colors to remove, while dark blue and black are the easiest. Flesh-colored tattoos, white ink, and permanent makeup are particularly tricky because the pigment in these colors can oxidize (turn black) when treated by laser. Oxidized pigment is no longer treatable by laser. Three types of lasers are currently used for tattoo removal: Q-switched ruby laser (694 nm), Q-switched neodymium-doped yttrium aluminum garnet (Nd: YAG) laser (532 nm, 1064 nm), and Q-switched alexandrite laser (755 nm). The Q-switched ruby and alexandrite lasers are useful for removing black, blue, and green pigments. The Q-switched 532 nm Nd: YAG laser can be used to remove red pigments and the 1064 nm Nd: YAG laser is used for removal of black and blue pigments. Besides laser, there are other, less commonly used ways to lighten tattoos such as dermabrasion (“sanding” away the top layer of skin using a motorized wire brush or abrader), ablative (non-tattoo) lasers (that burn off the entire top layer of skin), and surgical removal of the tattooed skin.[13]
This is worth noting that tattoo regret has become a major reason for removal in recent times. A tattoo regret means that a person feels regret and is dissatisfied with at least one of their tattoos after obtaining them. Studies have shown that tattoo regret rates have increased in recent years, as tattoos have become more popular and common.[10] In previous studies, it has been estimated that 16–44% of people with tattoos later regret at least one of their tattoos.[11] Tattoo regret is also correlated with acquiring one’s first tattoo at a younger age. The most common reason for regret was “not liking the tattoo anymore.” In addition, tattoo regret was compared according to age, gender, educational status, and tattooing practices. However, Kluger noted that the rate of tattoo regret may change in accordance with gender, age, interests, and even nationality. Tattoos performed by a professional tattoo artist lead to less tattoo regret as compared to tattoos performed by an amateur artist. A study indicated that current fashions and changing social attitudes toward tattoos may be primary reasons for tattoo regret. The main reasons are as follows: family or partner pressure, personality change, employment, changes of lifestyle or partner or poorly done tattoos. In another study, it was found that tattoo regret is related to getting the first tattoo at an earlier age, as well as to male gender, lower education level, and having the tattoo performed by an amateur or oneself.[11] A study performed among college students by Armstrong et al. revealed that 13% of them did not like their first tattoo, and 18% stated that their tattoo artist did not meet their expectations. Moreover, participants who had their tattoos applied on their upper extremities and face had higher regret rates of 29.3% and 44.1%, respectively.[14] It is likely that having tattoos on visible areas provides a greater inclination to regret. Yadav et al. also reported tattoo regret in patients of vitiligo and morphea, respectively [Figure 1], where these patients got tattoo from a local tattoo artist for camouflaging and later on ended in tattoo regret, as their disease got reactivated due to Koebnerzination in the disease.[12]
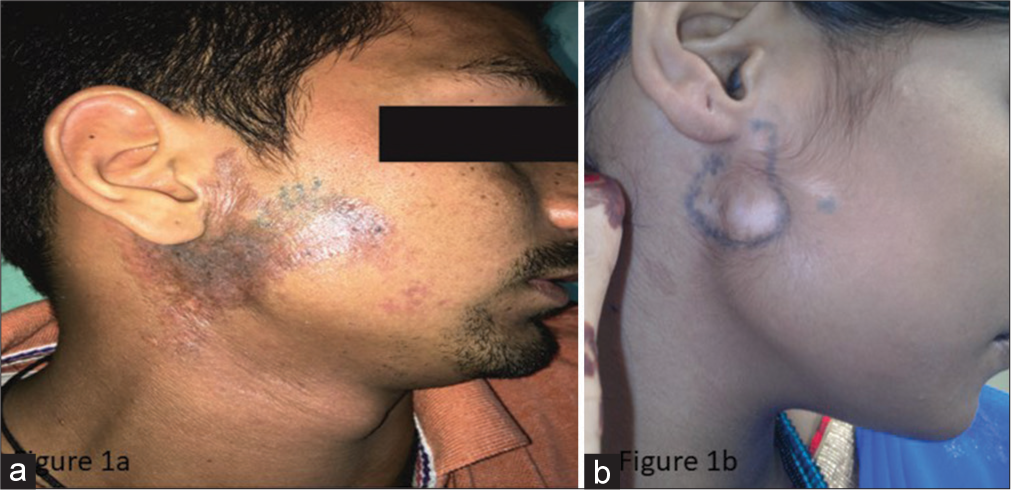
- (a) Tattooing over preexisting morphea and (b) vitiligo lesions.
There are certain advantages linked to tattooing as a camouflage technique also. It is especially useful in patients who do not achieve complete or immediate attractive results from dermatologic therapy for vitiligo. Micropigmentation gives rapid and instantaneous results in such cases. Micropigmentation is the deposition of minute and metabolically inert pigment granules into the dermis by electrically driven needles.[15] The pigments are deposited intradermally between the superficial and mid dermis, where they are permanently fixed intracellularly. The pigment which is used for micropigmentation is non-toxic, metabolically inert, and non-carcinogenic. It is a simple office procedure and cost effective and is not time consuming. It can be used for areas like the eyelid margin where other use of modalities is difficult. Micropigmentation is basically the esthetic use of tattooing in dermatology for camouflaging various skin conditions such as vitiligo, alopecia, madarosis, camouflaging scars due to burns, surgical defects, striae distensae, nevus depigmentosus, and idiopathic guttate hypomelanosis.[13] The decision for tattooing for therapeutic purposes, however, should be based on the proper selection of patient, stability of disease, the site of lesion, and other considerations. Therapeutic tattooing may also end up in tattoo regret due to difficulty in getting an exact color match or gradual color fading. Tattooing can also be utilized for therapeutic purposes in burns, surgical scars, etc.
Both motivations and regret for tattooing, in fact, address some psychological and psychiatric aspects of individuals or psycho-cultural features. Moreover, an exposed site of involvement like the face in patients should further stimulate to either assess the psychiatric impact in detail or seek an expert psychiatrist’s opinion if needed. Such patients need proper counseling to relieve their stress to the extent that they stay away from such harmful procedures.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- A survey on awareness and perception about tattoos among college students. Drug Inventions Today. 2018;10:2705-7.
- [Google Scholar]
- Prevalence of tattooing and knowledge about health risk associated with it among adolescent school students in Manipur, North-eastern India: A cross-sectional study. Int J Community Med Public Health. 2019;6:774-9.
- [CrossRef] [Google Scholar]
- Types of colourants used in tattoo and permanent make-up techniques, legal regulations, health, and psychological aspects of tattooing. Health Sci Rep. 2023;6:e1360.
- [CrossRef] [PubMed] [Google Scholar]
- Insights into worldwide interest in tattoos using Google trends. Dermatology. 2019;235:240-2.
- [CrossRef] [PubMed] [Google Scholar]
- The cultural heritage of tattooing: A brief history. Curr Probl Dermatol. 2015;48:1-5.
- [CrossRef] [PubMed] [Google Scholar]
- United States military service members and their tattoos: A descriptive study. Mil Med. 2013;178:921-5.
- [CrossRef] [PubMed] [Google Scholar]
- Tattoo practices in North-East India: A hospital-based cross-sectional study. J Cutan Aesthet Surg. 2016;9:172-6.
- [CrossRef] [PubMed] [Google Scholar]
- Tattoos: Demographics, motivations, and regret in dermatology patients. Indian J Dermatol. 2022;67:834.
- [CrossRef] [PubMed] [Google Scholar]
- Tattoo for camouflage: A new cause of tattoo regret. Indian Dermatol Online J. 2020;11:250-2.
- [CrossRef] [PubMed] [Google Scholar]
- College students and tattoos: Influence of image, identity, family, and friends. J Psychosoc Nurs Ment Health Serv. 2002;40:20-9.
- [CrossRef] [PubMed] [Google Scholar]







