Translate this page into:
Verrucous outgrowth on scalp

*Corresponding author: Manjit Kaur Rana, Department of Pathology, All India Institute of Medical Sciences, Bathinda, Punjab, India. drmrsmanjitkaur@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kapatia G, Jindal A, Bansal S, Rana MK. Verrucous outgrowth on scalp. CosmoDerma. 2024;4:93. doi: 10.25259/CSDM_89_2024
A 23-year-old female complained of an outgrowth on her scalp since birth. It was associated with bleeding whenever she scratched the lesion. On clinical examination, there was an outgrowth on the vertex area of the scalp with a verrucous surface measuring approximately 2 × 1 cm [Figure 1]. It was mildly erythematous and granulation like but non-tender. She has no specific personal or family history. The clinicians considered the possibilities of nevus sebaceous, wart, or hemangioma. A skin biopsy was taken from the lesion. Histological examination showed epidermis thrown into exophytic papillary fronds lined by dual cell layer-inner columnar epithelium and outer myoepithelial cell layer. The papillae were also focally lined by stratified squamous epithelium. The stroma of papillae and dermis showed dense infiltration by lymphoplasmacytic infiltrate [Figure 2]. No sebaceous gland hyperplasia or koilocytes or verrucous hyperplasia or dilated and congested blood vessels were seen.

- Verrucous outgrowth on scalp.
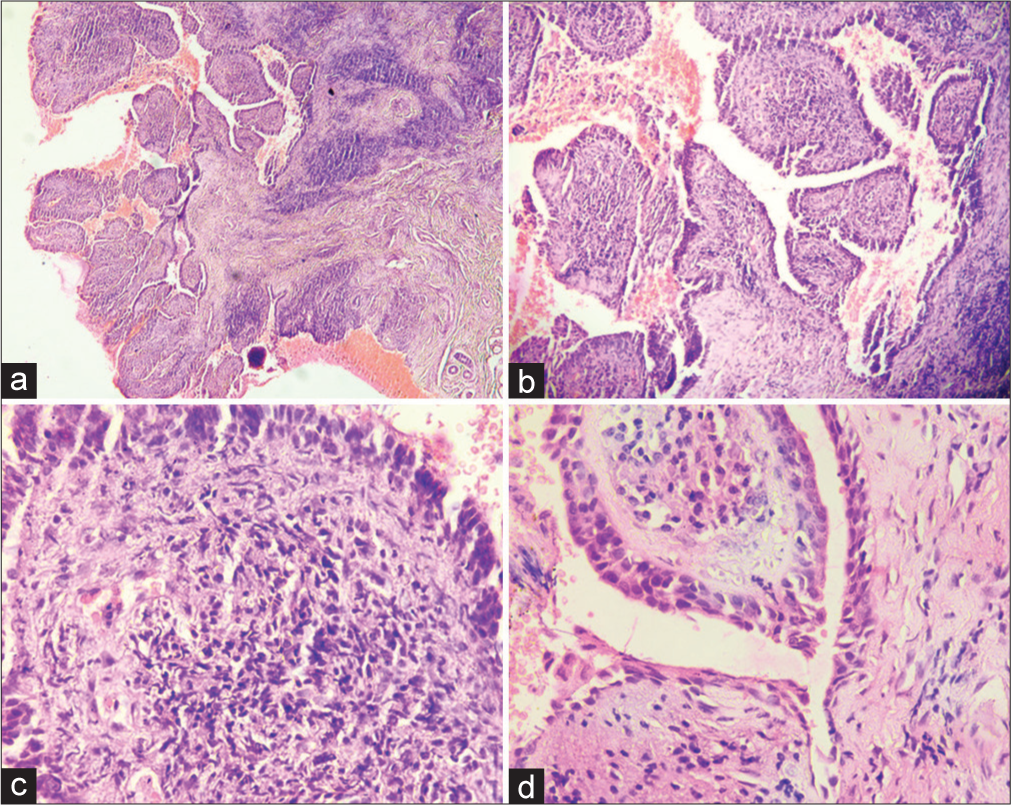
- (a) Low-power view shows epidermis thrown into exophytic papillary fronds and dense inflammatory infiltrate in the papillary stroma and dermis (H&E stain, ×40); (b) low-power view shows papillary fronds liner by dual cell layer and dense inflammation in the papillary stroma (H&E stain, ×100); and (c and d) high-power view shows the papillary fronds lined by dual cell layer and stroma shows dense lymphoplasmacytic inflammatory infiltrate (H&E stain, ×400).
WHAT IS THE DIAGNOSIS?
Answer:
Syringocystadenoma papilliferum (SCAP).
DISCUSSION
The SCAP is a rare benign adnexal tumor predominantly seen in childhood.[1] It is believed to arise from the apocrine or eccrine sweat glands.[1] In the majority of cases, it is present since birth or develops around infancy or before puberty.[1,2] It occurs rarely in adults. The SCAP occurs with equal frequency in both sexes.[3] It is characterized by asymptomatic skin to pink-colored lesions, which can present as a plaque, nodule, or linear lesion.[2,3] The tumor commonly involves the head-and-neck region.[2,4] The rare sites affected by SCAP include the pinna, external auditory canal, eyelid, buttock, vulva, and scrotum. The size of the lesion may vary from 1 cm to 4 cm in diameter.[1] It can be single or multiple. The SCAP is usually associated with other benign adnexal tumors, for example, nevus sebaceous, apocrine hidrocystoma, apocrine adenoma, clear cell syringoma, etc.[2] It can occur sporadically or as a secondary neoplasm. In 40% of cases, it arises from the underlying nevus sebaceous or organoid nevi.[3,5] Additional studies of SCAP may show both apocrine (positivity for gross cystic disease fluid protein 15 and 24 or zinc-2 glycoprotein) and eccrine differentiation (cytokeratin positivity).[3] The SCAP can transform into its malignant counterpart, syringocystadenocarcinoma papilliferum. Basal cell carcinoma has also been seen associated with SCAP in 10% of the cases. Squamous cell carcinoma may also develop in SCAP, but it is very rare as only two cases have been reported till now.[1] Clinical signs such as rapidly growing lesion or ulceration may be the indications of malignant transformation.[1] The treatment modalities for SCAP include laser, cryotherapy, or surgical excision.[2] Complete surgical excision and follow-up is the treatment of choice, as the tumor can recur due to incomplete excision and the associated risk of malignant transformation.[2] However, ablative CO2 laser therapy can be used in cases where surgical treatment is not possible. It is an effective treatment for SCAP, often resulting in excellent cosmetic outcomes and low recurrence rates.[6] Recently, it has been proposed that the pathogenesis of SCAP might be associated with BRAF V600 or HRAS mutations.[2] Drugs targeting these mutations may emerge as a newer modality of treatment for SCAP and its malignant counterpart. However, a biopsy of the lesion is necessary for the definitive diagnosis of SCAP, as it has variable clinical presentation which may lead to multiple differential diagnoses initially and also to rule out any malignant transformation of the tumor.[3,5] In the present case, the clinical possibilities included nevus sebaceous/wart/hemangioma but a diagnosis of SCAP was made on histopathological examination, thus making it a gold standard investigation for the diagnosis of adnexal tumors. The SCAP may arise in the background of nevus sebaceous, which may be missed if the biopsy is small.
Author’s contributions
GK was involved in the final evaluation of the case, manuscript drafting, editing, and revision. AJ took part in the evaluation of the case and manuscript drafting. MKR was involved in the final evaluation of the case. SB was involved in the management of the patient.
Ethical approval
The Institutional Review Board has waived the ethical approval for this study.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Syringocystadenoma papilliferum of the scalp in an adult male-a case report. J Clin Diagn Res. 2013;7:742-3.
- [CrossRef] [PubMed] [Google Scholar]
- Neonatal syringocystadenoma papilliferum: A case report. World J Clin Cases. 2021;9:4772-7.
- [CrossRef] [PubMed] [Google Scholar]
- Syringocystadenoma papilliferum of scalp: A rare case report. Int J Sci Study. 2015;2:182-5.
- [Google Scholar]
- Solitary syringocystadenoma papilliferum on the face: A rare case report with dermoscopic findings. Aust J Dermatol. 2020;61:e116-7.
- [CrossRef] [Google Scholar]
- Syringocystadenoma papilliferum of the scalp. Dermatol Online J. 2021;27:13030/qt7rh3260v.
- [CrossRef] [PubMed] [Google Scholar]
- Current diagnosis and treatment options for cutaneous adnexal neoplasms with apocrine and eccrine differentiation. Int J Mol Sci. 2021;22:5077.
- [CrossRef] [PubMed] [Google Scholar]





