Translate this page into:
Extra facial esthetic indications of botulinum toxin: A review

*Corresponding author: Gulhima Arora, Department of Dermatology, Mehektagul Dermaclinic, New Delhi, Delhi, India. gulhima@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Arora G, Singh N, Arora S. Extra facial esthetic indications of botulinum toxin: A review. CosmoDerma. 2024;4:32. doi: 10.25259/CSDM_259_2023
Abstract
Harnessing of the most potent neurotoxin, botulinum toxin (BTX) has been one of the most significant developments in the field of esthetics. Ever since its approval by the Food and Drug Administration in 2002 for the temporary improvement in the appearance of moderate-to-severe glabellar lines, BTX has been used for numerous off-label esthetic indications, the majority being facial indications. In this review, we intend to discuss the extra facial esthetic indications of BTX which include neck rejuvenation, improving shoulder contours, calf slimming, ankle slimming, and androgenetic alopecia. We have included essential tips for each indication.
Keywords
Botulinum toxin
Extra facial
Calf slimming
Androgenetic alopecia
Shoulder slimming
INTRODUCTION
Botulinum toxin (BTX) injection is the most commonly performed non-surgical esthetic procedure worldwide according to the report of 2022 released by the esthetic society.[1] A neurotoxin produced by the bacterium clostridium botulinum has seven distinct isoforms (BTX-A, B, C, D, E, F, and G), with BTX A and BTX B being commercially available.[2] It blocks the release of acetylcholine and several other neurotransmitters from presynaptic vesicles by deactivating the SNARE proteins.[2] Since its first description and the Food and Drug Administration approval in 2002 for temporary improvement in the appearance of moderate-to-severe glabellar lines, off-label use in face esthetics has often been discussed. In this article, we stress the versatility of its use for esthetic indications in areas other than the face.
NECK REJUVENATION
It is essential to address any signs of neck aging along with the face while managing signs of aging in this region. The use of BTX has gained popularity, as it is a quick and economical alternative to surgical procedures for patients, who are either young for facelift surgery or who are looking for a non-invasive procedure. The commonly observed esthetic deficiencies of the neck include horizontal neck wrinkles, crepey skin, sagging of skin with hanging folds, excessive adipose tissue causing double chins and/or poorly defined jawlines, and platysmal bands.[3,4]
Vertical bands
The platysma muscle is a large sheet of subcutaneous muscle. It extends three finger breadths above and parallel to the lower border of the mandible, one finger breadth posterior to the depressor anguli oris, and all the way down over the cervicomental angle and anterior neck to the upper border of the clavicle, and posteriorly to the anterior border of the sternocleidomastoid.[5]
Platysmal contraction blunts the cervicomental angle. A lax platysma shall hence result in an obscure, ill-defined jawline. In addition, bands formed on its contraction, known as platysmal bands, are the result of this persistently active muscle trying to support the sagging deeper neck and floor of the mouth structures. The anterior edges of the muscle lose tone and separate over time to protrude anteriorly forming the “turkey neck” deformity.[6]
Injection technique
The vertical neck bands are made prominent by asking the patient to clench the teeth and depress the lateral oral commissure [Figure 1]. An individual band is grasped between the thumb and index finger of the non-dominant hand and 1–2 U of BTX A (100 U BTX A is diluted with normal saline of 2.5 mL) is injected 1.5–2 cm apart directly into the belly of the muscle. Three to five sites per band are usually enough. A total of 15–20 U BTX A are recommended for the neck.[7]
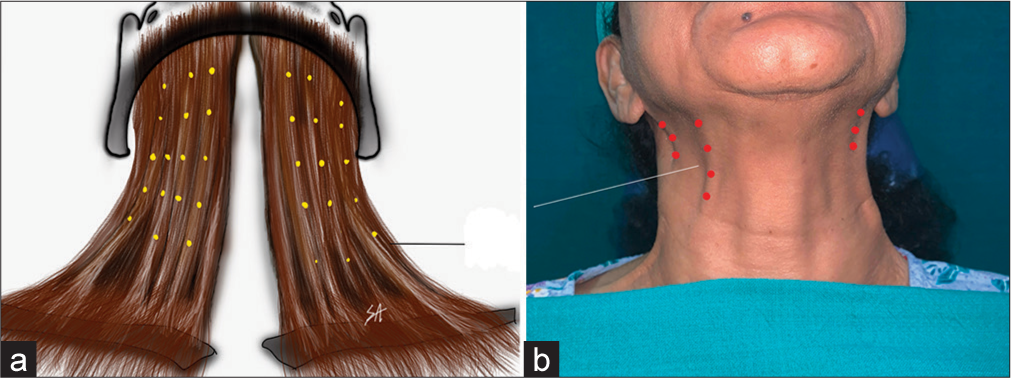
- Platysma bands: (a) Platysma anatomy with injection points (yellow dots) and (b) surface anatomy with injection points (red dots).
Complications
Injection-related transient complications such as erythema, bruise, and pain can occur.
A deeper placement of a needle during injection can affect pharyngeal and laryngeal muscles, which can lead to dysphagia and dysphonia.
Practice tip
Mark the bands in a sitting position
Hold the muscle band between the thumb and index finger
Inject while the patient is semi-reclining
Horizontal injections into the band and not vertically down avoid direct deeper diffusion.
Horizontal lines or venus rings
Horizontal neck lines present as linear depressions or furrows, which occupy the anterior half of the neck [Figure 2].[8] These form as a result of the pleating of overlying skin perpendicular to the underlying platysma. The BTX has been used to relax the platysma and smoothen neck bands and lines. The horizontal neck wrinkles are not entirely caused by aging, as they are often observed in children and young adults.[9,10] However, age-related skin laxity often worsens these lines.[9]
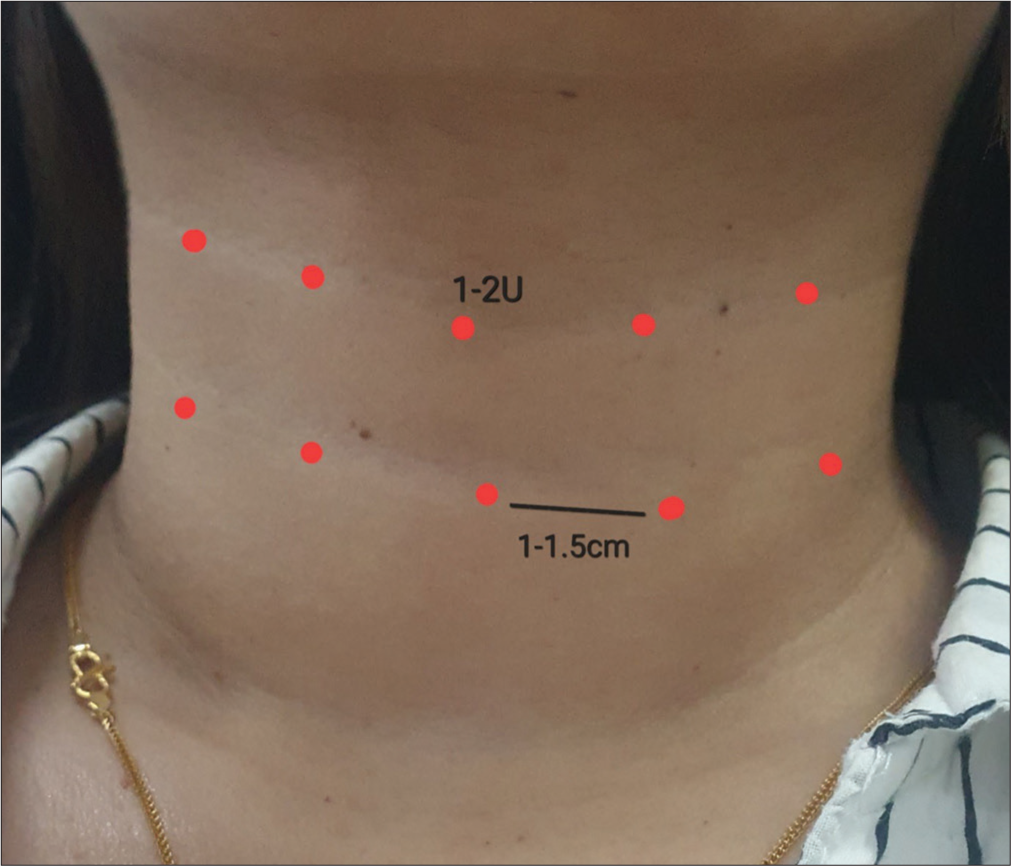
- Horizontal neck lines: 1–2 U of botulinum toxin A is injected at 8–10 points (red dots) 1–1.5 cm apart.
Technique of injection
The 100 U BTX A is diluted with normal saline of 2.5 mL, and 1–2 U is placed into each injection point using a 30-gauge needle. Injections are performed at points 1–1.5 cm apart along the horizontal lines [Figure 2]. The total maximum injected dose of BTX A has been 15 units for each horizontal neckline in a single session.[11]
Complications
The injection-related transient complications such as erythema, bruise, and pain can occur.
In rare cases, if the injection is placed deep and extremely lateral, the toxin can weaken the sternocleidomastoid muscle leading to difficulty in keeping the neck still and erect.
High dose of toxin and deeper placement of needle can affect pharyngeal and laryngeal muscles which can lead to dysphagia and dysphonia.
Microbotox
Microbotox is a term coined in 2001 to describe the technique of delivering multiple intradermal or subdermal injections of diluted onabotulinumtoxinA into the overlying skin envelope and superficial layer of the facial and neck muscles.[12,13]
Mechanism of action
Microbotox injections weaken the superficial fibers of the platysma, while the deeper muscle fibers continue to function and exert their muscle pull inward and upward creating a more snug apposition of the platysma to the underlying neck structures. This creates a more defined cervicomental angle and the illusion of lifting the jowls and jawline. This is called the “platysma effect.”[12]
This technique also specifically targets the sweat and sebaceous glands as well as the superficial fibers of the facial muscles that take attachment to the undersurface of the dermis.
Microbotox of the neck is suited for patients, who suffer from mild neck laxity and jowling, crepey neck, horizontal neck lines, and vertical banding.[12]
Technique of injection
To prepare the Microbotox solution, a 100 U vial of BTX A is reconstituted with 2.5 mL of saline (standard dilution). Further, 0.5 mL of BTX A is withdrawn from this vial and a further 0.5 mL of lidocaine (0.5%) with or without adrenaline is then drawn into the syringe to make it up to 1 mL volume. This gives a concentration of 20 units of BTX per mL.
If the platysma is bulky (thicker necks): 28 units/ml. Prepare by drawing 0.7 ml (28 units) from a vial with standard dilution and top it up with 0.3 ml lidocaine (0.5%) with or without adrenaline.[12]
The injection is given in a semi-reclined position with the neck arched upward to make the skin taut. Additionally, stretching between finger maintains the tautness. A 30–32 G needle is used with the bevel pointed downward, and BTX A is injected 8–10 mm away with extreme caution to just penetrate the needle into the skin as superficially as possible [Figure 3].
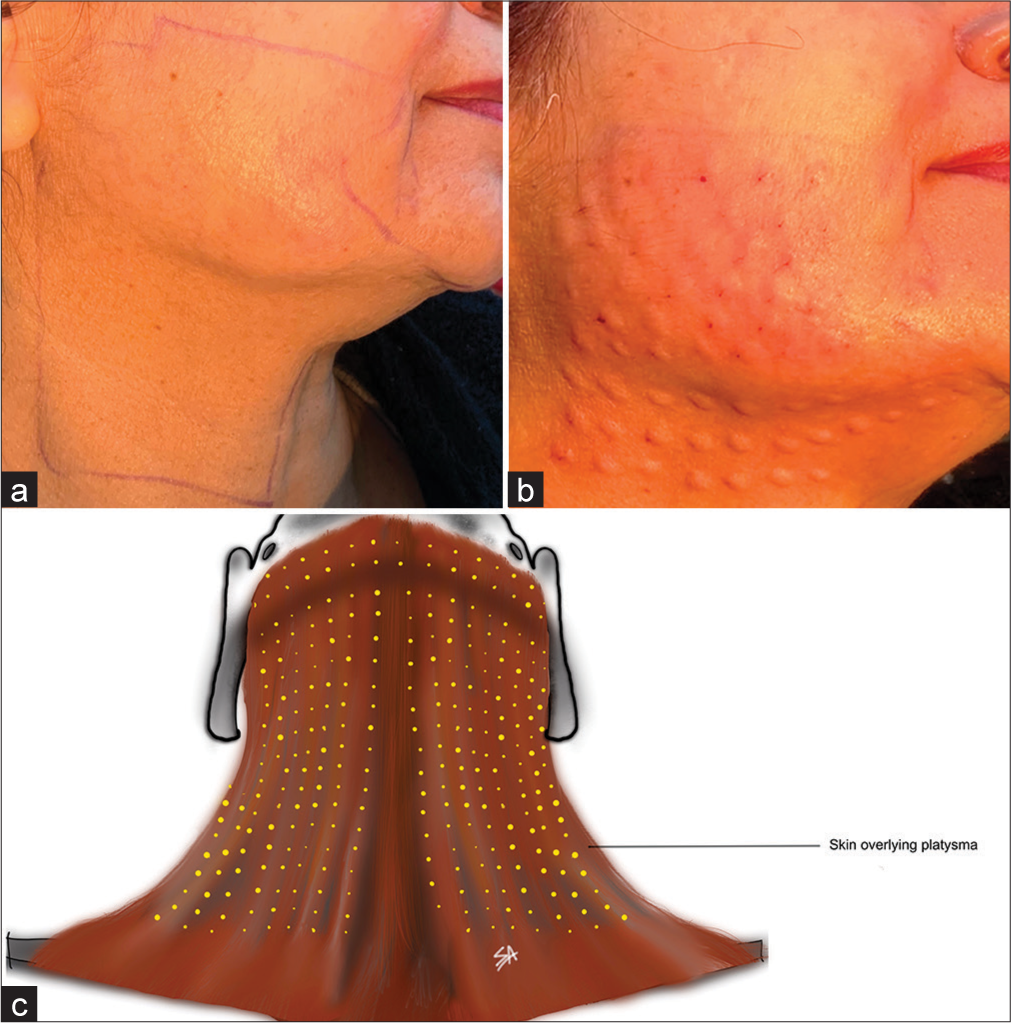
- Microbotulinum toxin: (a) Surface marking for platysma on one side, (b) superficial injection blebs visible upon toxin infiltration, and (c) neck with injection points (yellow dots) for reference on the entire neck and inferior border of mandible.
In the average lower face and neck, 1 mL of microbotox is used to cover the entire area of one-half of the lower face and neck.
An alternative to this technique has been described by Calvani et al. as the “superficial injection needling botulinum” technique. A higher concentration of onabotulinumtoxinA (50 U in a 0.8-mL syringe) is delivered intradermally using an electrical needling pen to a depth of 3–3.5 mm.[14]
Practice tip
Keep the syringe angled to <15° to the surface.
Insert the needle bevel deep.
Complications
The injection-related transient complications such as erythema, bruise, and pain can occur.
An incorrect injection technique can lead to weakness of depressor anguli oris leading to smile asymmetry.
In rare circumstances, if the injection is placed deep, the toxin may diffuse into the sternocleidomastoid muscle, which can lead to a floppy neck; and difficulty in keeping the neck still and erect.
A high dose of toxin and deeper placement of the needle can lead to pharyngeal and laryngeal muscle weakness causing dysphagia and dysphonia.
ANDROGENETIC ALOPECIA
Androgenetic alopecia is a common form of alopecia with a multifactorial etiology. Orentreich proposed that the miniaturization of hair follicles occurs in genetically predisposed androgen-sensitive hair follicles. This androgenetic theory states that the miniaturization of hair follicles results from the action of dihydrotestosterone (DHT).[15,16] A low oxygen environment resulting from microvascular insufficiency at the follicular level promotes the conversion of testosterone to DHT.[17] Few experimental studies suggest that subcutaneous blood flow in the scalp of a patient with male-pattern baldness was greatly reduced as compared to controls.[18] The relatively avascular galea aponeurotica underlying the frontal and vertex as compared to the better vascularized temporal and occipital areas underlined by muscles may also be responsible for this microvascular insufficiency.[19] This relative microvascular insufficiency hence adds to other factors leading to the miniaturization of hair follicles.[20]
Mechanism of action of BTX A for androgenetic alopecia
The BTX A relaxes the muscle thus reducing pressure on the musculocutaneous and perforating vasculature, thereby increasing the blood supply and transcutaneous pO2. This increased blood flow can also lead to the washing out of accumulated DHT, thereby reducing the signal for miniaturization of hair follicles. Furthermore, a high concentration of oxygen can stimulate the hair follicle into the growth phase resulting in hair regeneration.[21,22]
Technique of injection
The BTX A 100 U diluted in 1 mL normal saline is injected intramuscularly at 30 different sites; 5 U at each site resulting in a total of 150 U in the frontalis, occipitalis, temporalis, and periauricular muscles [Figure 4],[22] 30–32G needles are preferred.
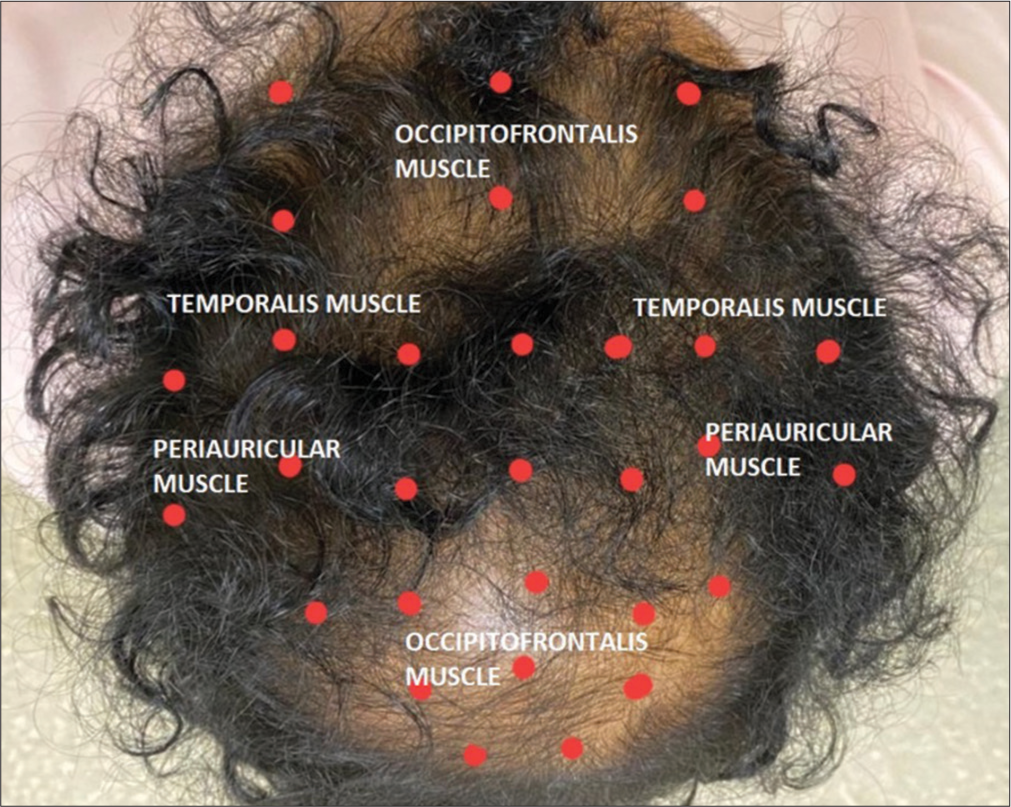
- Androgenetic alopecia: 30 points (red dots) to be injected with 5 U of botulinum toxin A at each point. The muscles that are targeted are occipitofrontalis, temporalis, and periauricular muscles.
Complications
None reported, but suboptimal results may be experienced, as this modality does not tackle the androgenetic pathway.
Practice tip
Ensure adequate topical anesthesia, as these volumes are painful on the scalp.
CALF CONTOURING
Non-surgical body contouring is now increasingly popular. Chubby and muscularly shaped legs are a cause of lower confidence among females. These are known colloquially as radish legs. Gastrocnemius and soleus muscles determine the posterior contour of the legs. The medial head of the gastrocnemius muscle forms a prominent contour medially in the posterior aspects of the legs in Asian women.[23] Surgical interventions such as muscle resection, liposuction, selective neurectomy or radiofrequency have been observed to produce ankle contractures, painful scars, and unpredictable outcomes.[24] The BTX A is used to contour the legs, and as a therapy, is a simple alternative to calf reduction surgery without interrupting the daily life routine.[25]
Technique of injection
Assess the degree to which the gastrocnemius muscle is contributing to the calf bulge. A pinch test to differentiate it from fat bulges is useful.[26] Determine the calf bulge type; a uniform or medial bulge due to the relevant gastrocnemius head bulk. The BTX A in 2.5 mL dilution is injected in the tip-toe prone position using a 1-inch 23 G needle. Authors prefer using a 24 G IV cannula needle, which provides enough depth and is less painful. Although numerous injection points have been described targeting the most bulky area and avoiding underdosing is the common rule[27] [Figure 5]. Dose depends on the bulk of muscle hypertrophy, and usually, 30–200 U are injected on each side.[25] Liu et al., have proposed a scoring system to determine the bulk volume and pattern to calculate the total dose needed.[28] Three to six intramuscular injections 1.5–2 cm apart are recommended to be administered in the most prominent part of the medial and lateral head of the gastrocnemius.
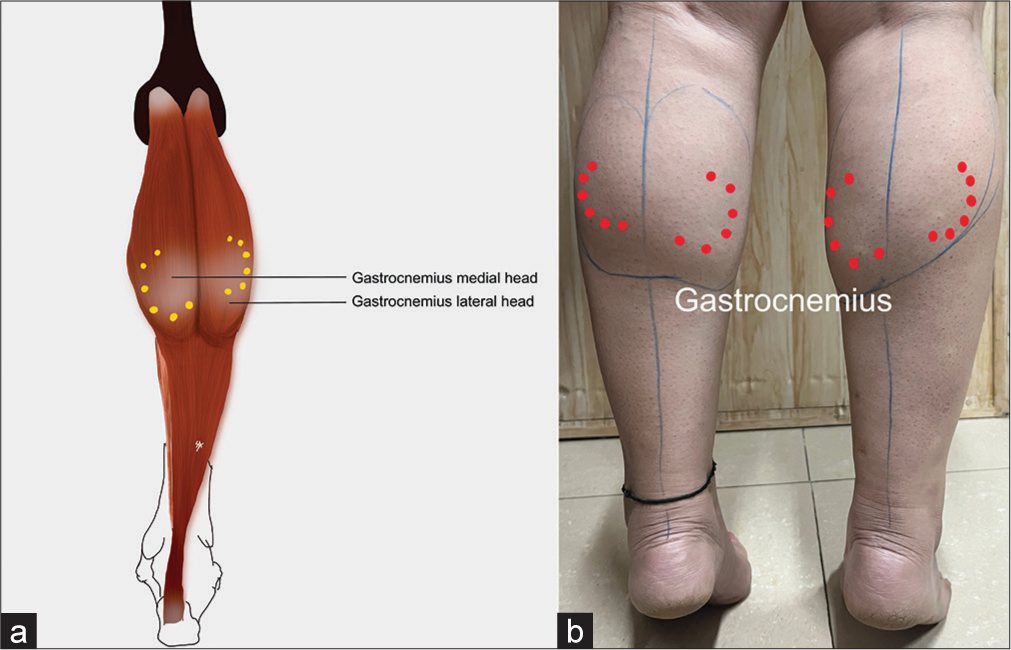
- Calf slimming effect: (a) Anatomy of gastrocnemius with injection points (yellow dots) for reference, and (b) three to six intramuscular injections of botulinum toxin A is given 1.5–2 cm apart administered into the most prominent part of gastrocnemius (red dots).
Complications
At higher doses, it can lead to calf muscle weakness resulting in gait disturbance and fatigue after walking or running.
Practice tip
Adequate topical anesthesia must be used. Use a thinner cannula to ensure adequate depth and less painful injections
Gastrocnemius is a bulky muscle, avoid underdosing.
ANKLE CONTOURING
With the changing perception of beauty, a thin ankle is considered a sign of beauty in modern times. Since the skin around the ankles has a very low fat content, the muscle layer (soleus) should be reduced to obtain thin ankles.[29] The BTX A is a simpler and safer alternative to surgery for contouring large ankles.
Technique of injection
Each soleus muscle is injected with 50 units of BTX A in 1.2 mL diluent, as an intramuscular injection on both sides of the ankle [Figure 6]. A total dose of 100 units of BTX was administered to each ankle.[30]

- Ankle contouring: (a) Anatomy of soleus with injection points (yellow dots) for reference and (b) three to six intramuscular injections of botulinum toxin A is given on both sides of each soleus muscle (red dots).
Complications
If a higher dose of toxin is used, there may be ankle weakness and difficulty in walking and running.
Practice tip
Attempt this indication in combination with gastrocnemius
This muscle lies deeper into the gastrocnemius. It contributes to the lateral calf/ankle bulk and is accessible and injected along its lateral borders.
SHOULDER SLIMMING
Smooth shoulder lines are considered a desirable feature in females. Hypertrophy of the trapezius muscle leads to a broad-looking shoulder and a shorter neck, which impacts the patient’s attractiveness and perception of beauty. The BTX A can create smooth and neat contours by volume reduction of the trapezius muscle.[31] This also gives a perception of a longer neck.
Mechanism of action
The BTX helps to relax the hypertrophied trapezius muscles creating smooth contours, which in turn helps to improve the neck length.
Technique of injection
The upper border of the trapezius is marked out. The most prominent strip of the upper portion of the trapezius muscle is chosen [Figure 7]. Anatomical studies on cadavers and thereafter their clinical application have demonstrated a common area on the muscle that provides the best results for toxin administration. Lee et al. marked out a line from the occipital protuberance to the lateral most portion of the acromion, on the superior most portion of trapezius and divided it into fifths. The area covered by the fourth region has been shown to contain the maximum number of neuromuscular junctions followed by the third region.[32] Bae et al. arrive at a similar region on a line joining the seventh spinous process to the acromion.[33] Toxin injection in this region is the most beneficial. Five to six points, 2 cm apart are injected with 5–10 U on each side, for a total of 30–50 U of BTX A. Depth of injection recommended is 13 mm with a 27–30 G needle[34,35] [Figure 5]. Ultrasound guidance may also be used to determine the most hypertrophied area of the muscle.[36]

- Shoulder slimming effects: (a) Anatomy of trapezius with injection points (yellow dots) for reference; (b) botulinum toxin A is injected at five or six points (red dots) 1-2 cm apart, each point receiving 5-10 U of the toxin.
Complications
If the BTX is injected extremely close to the neck, it can lead to neck muscle weakness.
The extreme lateral injection point can lead to diffusion of BTX to the origin of the deltoid muscle, which may cause difficulty in shoulder joint extension.
Regular injection of BTX into the muscle leads to neurogenic atrophy with muscle mass loss.[35]
Practice tip
Mark the bulkiest portion of the trapezius from the frontal view
Mark the injection points from the posterior view.
Avoid the descending margin of the trapezius.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- The aesthetic society releases annual statistics revealing significant increases in face, breast and body in 2021. Available from: https://www.prnewswire.com/news-releases/the-aesthetic-society-releases-annual-statistics-revealing-significant-increases-in-face-breast-and-body-in-2021-301522417.html [Last accessed on 2023 Mar 05]
- [Google Scholar]
- Botulinum toxin-know the product before injecting. Cosmo Derma. 2021;1:56.
- [CrossRef] [Google Scholar]
- Anatomy and physiology of the aging neck. Facial Plast Surg Clin N Am. 2014;22:161-70.
- [CrossRef] [PubMed] [Google Scholar]
- A classification of facial wrinkles. Plast Reconstr Surg. 2001;108:1735-50. discussion 1751-2
- [CrossRef] [PubMed] [Google Scholar]
- Microbotox of the lower face and neck: Evolution of a personal technique and its clinical effects. Plast Reconstr Surg. 2015;136:92S-100.
- [CrossRef] [PubMed] [Google Scholar]
- The anatomical basis for common cosmetic anterior neck deformities. Ann Plast Surg. 1979;2:381-8.
- [CrossRef] [PubMed] [Google Scholar]
- Where and how to use botulinum toxin on the face and neck-indications and techniques. Cosmo Derma. 2021;1:17.
- [CrossRef] [Google Scholar]
- The aging neck: A diagnostic approach to surgical and nonsurgical options. J Cosmet Laser Ther. 2013;15:56-64.
- [CrossRef] [PubMed] [Google Scholar]
- Correction of horizontal neck lines: Our preliminary experience with hyaluronic acid fillers. J Cosmet Dermatol. 2018;17:590-5.
- [CrossRef] [PubMed] [Google Scholar]
- Development and validation of a photonumeric scale for evaluation of transverse neck lines. Dermatol Surg. 2016;42:S235-42.
- [CrossRef] [PubMed] [Google Scholar]
- A prospective observational study of the effectiveness and safety of botulinum toxin in the horizontal neck lines. Aesthetic Plast Surg. 2018;42:1370-8.
- [CrossRef] [PubMed] [Google Scholar]
- Facial rejuvenation without facelifts-personal strategies. Regional conference in dermatological laser and facial cosmetic surgery 2002 In: Hong Kong. 2002.
- [Google Scholar]
- Skin resurfacing with Microbotox and the treatment of keloids. (Series in cosmetic and laser therapy) In: Benedetto AV, ed. Botulinum toxins in clinical aesthetic practice (2nd ed). Informa Healthcare; 2011. p. :190-205. Available from: http://informahealthcare.com/doi/abs/10.3109/9781841847559.006 [Last accessed on 2023 Nov 14]
- [CrossRef] [Google Scholar]
- Personal technique of microinfiltration with botulin toxin: The SINB technique (superficial injection needling botulinum) Plast Surg (Oakv). 2019;27:156-61.
- [CrossRef] [PubMed] [Google Scholar]
- Botulinum toxin beyond aesthetics in dermatology. Cosmo Derma. 2022;2:15.
- [CrossRef] [Google Scholar]
- Autografts in alopecias and other selected dermatological conditions. Ann N Y Acad Sci. 1959;83:463-79.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of male pattern baldness with botulinum toxin: A pilot study. Plast Reconstr Surg. 2010;126:246e-8.
- [CrossRef] [PubMed] [Google Scholar]
- Transcutaneous PO2 of the scalp in male pattern baldness: A new piece to the puzzle. Plast Reconstr Surg. 1996;97:1109-16.
- [CrossRef] [PubMed] [Google Scholar]
- The surgical repair of traumatic defects of the scalp. Clin Plast Surg. 1982;9:131-44.
- [CrossRef] [Google Scholar]
- Conversion of testosterone-1,2,3H to Androstenedione-3H in the isolated hair follicle of man. J Clin Endocrinol Metab. 1972;34:512-5.
- [CrossRef] [PubMed] [Google Scholar]
- A small dose of botulinum toxin A is effective for treating androgenetic alopecia in Chinese patients. Dermatol Ther. 2019;32:e12785.
- [CrossRef] [Google Scholar]
- A pilot study to evaluate effectiveness of botulinum toxin in treatment of androgenetic alopecia in males. J Cutan Aesthetic Surg. 2017;10:163.
- [CrossRef] [PubMed] [Google Scholar]
- Endoscope-assisted calf reduction in Orientals. Plast Reconstr Surg. 2000;106:713-8. discussion 719-20
- [CrossRef] [Google Scholar]
- Calf reduction by partial resection of gastrocnemius using a suction-assisted cartilage shaver. Plast Reconstr Surg. 2020;145:734e-43.
- [CrossRef] [PubMed] [Google Scholar]
- Botulinum toxin A for aesthetic contouring of enlarged medial gastrocnemius muscle. Dermatol Surg. 2004;30:867-71.
- [CrossRef] [PubMed] [Google Scholar]
- Undesirable outcomes from liposuction of the calves and ankles, what to avoid? Med Arch. 2020;74:396.
- [CrossRef] [PubMed] [Google Scholar]
- Botulinum toxin injections for leg contouring in east Asians. Dermatol Surg. 2020;46:S62-70.
- [CrossRef] [PubMed] [Google Scholar]
- Classification of gastrocnemius muscle hypertrophy for personalized botulinum toxin type A treatment. J Cosmet Dermatol. 2024;23:90-8.
- [CrossRef] [PubMed] [Google Scholar]
- Documentation and three-dimensional modelling of human soleus muscle architecture. Clin Anat. 2003;16:285-93.
- [CrossRef] [PubMed] [Google Scholar]
- Soleus muscle reduction with botulinum toxin type A injection for ankle contouring. Plast Reconstr Surg Glob Open. 2021;9:e3565.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy and safety of botulinum toxin type A injection in patients with bilateral trapezius hypertrophy. Aesthetic Plast Surg. 2018;42:1664-71.
- [CrossRef] [PubMed] [Google Scholar]
- Botulinum toxin injection-site selection for a smooth shoulder line: An anatomical study. BioMed Res Int. 2017;2017:3092720.
- [CrossRef] [PubMed] [Google Scholar]
- Accessory nerve distribution for aesthetic botulinum toxin injections into the upper trapezius muscle: Anatomical study and clinical trial: Reproducible BoNT injection sites for upper trapezius. Surg Radiol Anat. 2018;40:1253-9.
- [CrossRef] [PubMed] [Google Scholar]
- Changes in contractile properties of muscles receiving repeat injections of botulinum toxin (Botox) J Biomech. 2011;44:39-44.
- [CrossRef] [PubMed] [Google Scholar]
- Onabotulinumtoxin A for correcting trapezius muscle hypertrophy in Asian women. J Cosmet Dermatol. 2022;21:2677-9.
- [CrossRef] [PubMed] [Google Scholar]
- Ultrasound-guided five-point injection of botulinum toxin for patients with trapezius hypertrophy. J Orthop Surg. 2021;16:634.
- [CrossRef] [PubMed] [Google Scholar]






