Translate this page into:
Scleromyxedema presenting after treatment of multiple myeloma

*Corresponding author: Pradeep S. Nair, Department of Dermatology and Venereology, Government Medical College, Thiruvananthapuram, Kerala, India. dvmchtvm@yahoo.co.in
-
Received: ,
Accepted: ,
How to cite this article: Nair PS, Kabilan T, Sudhesan A. Scleromyxedema presenting after treatment of multiple myeloma. CosmoDerma. 2024;4:10. doi: 10.25259/CSDM_266_2023
Dear Sir,
Scleromyxedema (SM) is a rare chronic progressive disorder of unknown etiology characterized by fibrosis of the dermis and dermal mucin deposition. There may be an association with a monoclonal paraproteinemia usually of the immunoglobulin G kappa type and sometimes even overt multiple myeloma.[1]
A 64-year-old female diagnosed with multiple myeloma, was treated with lenalidomide (20 mg/day) for six months. At that time, there were no skin lesions. Following remission lenalidomide was stopped. After 2 months of stopping treatment, the patient presented with pruritic papules on the neck and upper back. The lesions first started on the neck and then spread to the upper back. On examination, there were multiple discrete and confluent skin-colored waxy lichenoid papules and plaques with “peau d’orange” appearance distributed on the lower posterior neck, upper back, and interscapular region [Figure 1]. On palpation, there was induration of the skin. The rest of the body was not affected, and there was no lymphadenopathy. There were no systemic features.

- Waxy lichenoid papules and plaques with “peau d’orange” appearance.
Hemoglobin was 9 mg%, peripheral smear showed microcytic anemia, and erythrocyte sedimentation rate was 50 mm in the first hour. Viral markers were negative. Thyroid function tests were normal. Bence–Jones protein was negative, and serum electrophoresis was normal. Bone marrow examination was normal. A hematological evaluation did not show current features of paraproteinemia or multiple myeloma. Investigations for systemic involvement were normal. A skin biopsy from the waxy papule showed pale areas in between the collagen bundles with mucin deposition and prominent fibroblasts [Figure 2]. A colloidal iron stain highlighted mucin deposition in the upper dermis [Figure 3]. We made a final diagnosis of SM. The patient was treated with lenalidomide (10 mg daily) for three months and showed prompt response [Figure 4]. There were no adverse reactions with lenalidomide. There was no relapse after a 6-month follow-up.
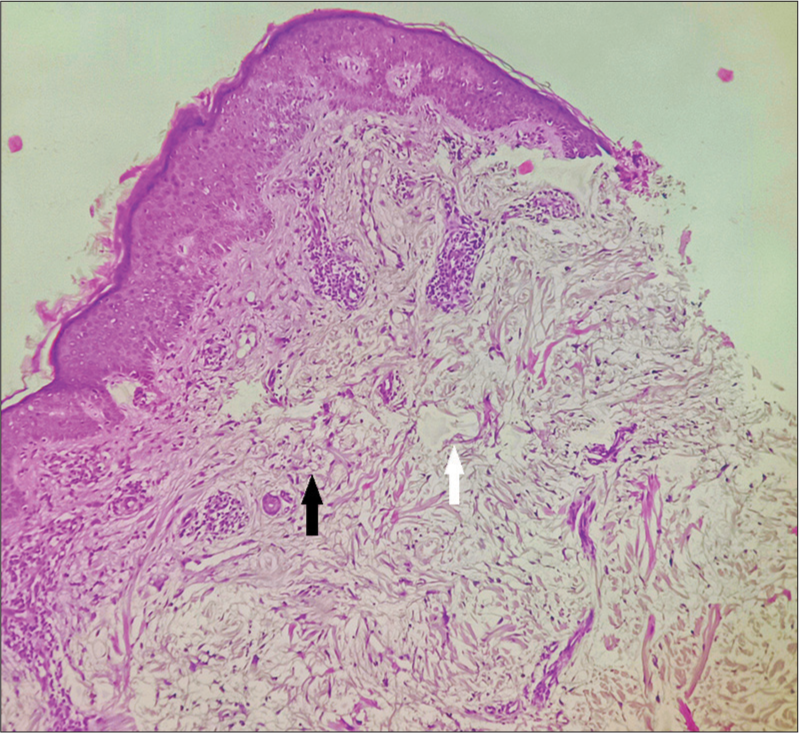
- Skin biopsy showing numerous fibroblasts and pale areas in the upper dermis, H and E × 100.
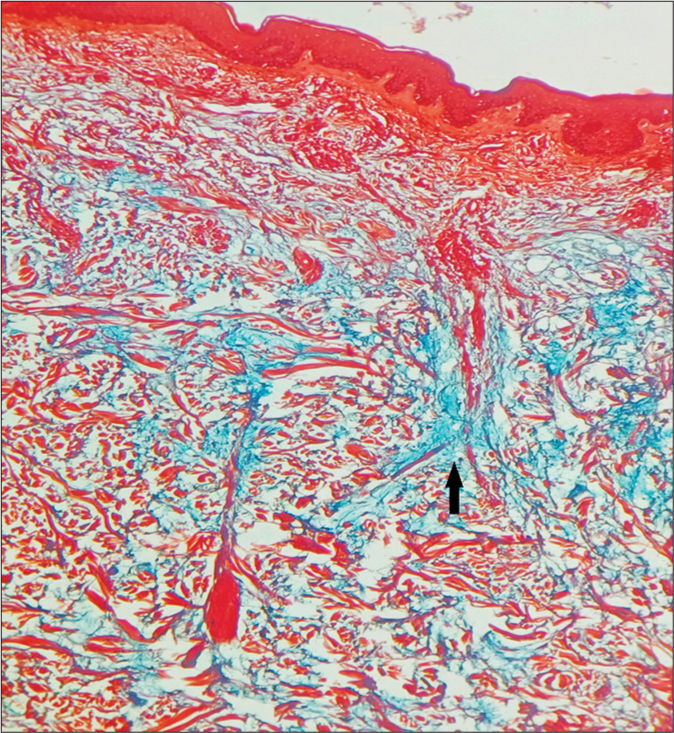
- Colloidal iron stain highlighting mucin deposition in upper dermis (arrows), Colloidal iron × 100.

- Prompt response after treatment with lenalidomide for 3 months.
The SM presents as generalized lesions or discrete localized (lichen/papular myxedematosus) lesions. Our case confers to the latter type. Face is another common site to be involved (not in our case) giving a “bovine facies.” Involvement of the skin on the upper back and shoulders throws the skin into longitudinal folds known as “Shar-Pei” sign. Waxy papules and plaques on the knuckles may show a central depression designated as the “doughnut sign”. The axillary and pubic hair may be sparse. Mucosa is usually not involved. The generalized type may be associated with paraproteinemia and multiple myeloma. However, there is considerable overlap, and localized types may evolve into generalized type. Muscular weakness, contractures, pulmonary involvement, esophageal dysmotility, central nervous system involvement, and rarely renal and cardiac involvement are the systemic features, none present in our case.[2]
Increased hyaluronate production and fibroblast production are the contributory factors in the pathogenesis of SM. It is postulated that fibroblast precursors from the bone marrow migrate to the skin and are deposited there producing mucin.[3] Hence, the histopathological hallmark is mucin deposition in the upper dermis, which gives the waxy appearance to the skin lesions and the sclerosis of the skin. An important histological differential diagnosis is nephrogenic systemic fibrosis (NSF). The involvement in SM is in the upper dermis while NSF involves the lower dermis and the septa of the subcutaneous tissue.
Localized SM may undergo self-healing, but frequent follow-up is necessary to detect paraproteinemias. There are no evidence-based treatment modalities for SM due to its rarity. The drugs tried are melphalan, systemic steroids, intravenous immunoglobulin (IVIG), interferon alfa, psoralen + ultraviolet A (PUVA), electron beam therapy, extracorporeal photopheresis, thalidomide, and lenalidomide (given in our patient).[4] The IVIG has shown excellent response in a recent case series where there was considerable improvement in both the skin lesions and systemic symptoms.[4] Autologous peripheral blood stem transplantation and bortezomib are new promising modalities.[5] In the usual case when investigating for SM, we may detect paraproteinemia and rarely multiple myeloma, but in our case, the patient was a treated case of multiple myeloma, but later developed SM when therapy for multiple myeloma was stopped, and the patient also did not have evidence of paraproteinemia or multiple myeloma during the presentation of SM to us. When the patient presented to us, there was no evidence of multiple myeloma relapse. However, the skin lesions were of short duration (two months) when presenting to us, and it is possible if the patient consulted for the skin lesions very late, the patient could have also presented with features of paraproteinemia or multiple myeloma. This is the highlight of this case, and thus we are reporting this case. We could not come across any similar reports to the best of our knowledge.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Scleromyxedema: A multicentric study of characteristics, comorbidities, course and therapy in 30 patients. J Am Acad Dermatol. 2013;69:66-72.
- [CrossRef] [PubMed] [Google Scholar]
- Scleromyxedema and the dermo-neuro syndrome: Case report and review of literature. J Cutan Pathol. 2012;39:508-17.
- [CrossRef] [PubMed] [Google Scholar]
- Histopathological characteristics of scleromyxedema: A study of a series of 34 cases. J Am Acad Dermatol. 2016;74:1194-200.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical characteristics and treatment outcomes of scleromyxedema: A 10-year retrospective survey. Case Rep Dermatol. 2022;14:178-83.
- [CrossRef] [PubMed] [Google Scholar]
- Scleromyxedema treatment: A systemic review and update. Int J Dermatol. 2020;59:1191-201.
- [CrossRef] [PubMed] [Google Scholar]





