Translate this page into:
“Acne” terminology in dermatology

*Corresponding author: Vishal Gaurav, Department of Dermatology and Venereology, All India Institute of Medical Sciences, New Delhi, India. mevishalgaurav@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Najeeb A, Gaurav V. “Acne” terminology in dermatology. CosmoDerma. 2024;4:4. doi: 10.25259/CSDM_244_2023.
INTRODUCTION
The term “acne” finds its origins in the Greek word “acme” (plural: akmas), signifying “a point” or “a peak,” metaphorically referring to puberty or the prime of life. It has also been used to refer to the crisis of a disease. The initial use of the term “acme” can be traced back to Cassius in the third century C.E. However, the term “acne” (plural: acmas) came into existence due to a transcription error during the translation from Greek to Latin when “acmas” was mistakenly written as “acnas.” The term “acne” was first used by Aetius Amidenus in the sixth century C.E.[1] In Ayurveda, acne is called “yauvanapidika” or “mukhdosha.”[2]
Nonetheless, the word “acne” has been employed as both a prefix and suffix for acne-related and -unrelated conditions, often resulting in misnomers. For instance, “acne aestivalis” is a photodermatosis and unrelated to acne vulgaris. Similarly, the term “acne agminata” (lupus miliaris disseminatus faciei [LMDF]) is a misnomer, as it neither represents a variant of acne vulgaris nor an agminate lesion but rather a granulomatous dermatosis involving the face. Often such a nomenclature can create confusion leading to mistreatment. Hence, this article attempts to classify them as acne-related and -unrelated entities.
For this article, we have endeavored to compile a comprehensive list of well-known and less well-known conditions in dermatology texts that incorporate the term “acne” in their nomenclature. Details regarding their etiopathogenesis, clinical features, and management were searched and compiled as appended below.
ACNE-RELATED TERMS
Acne vulgaris
Common acne or acne vulgaris is a disorder of the pilosebaceous unit presenting with non-inflammatory open and closed comedones and inflammatory papules, pustules, nodules, and cysts involving the face, back, and chest. The usual presentation is in adolescence, due to the spike of androgens, especially dehydroepiandrosterone (DHEAS) causing increased sebum production. Cutibacterium acnes (formerly Propionibacterium acnes) also play an important role in the pathogenesis of acne. Treatment depends on the severity and includes topical (retinoids, benzyl peroxide, and antibiotics) and oral (antibiotics and retinoids) agents.[3]
Variants based on morphology
The common clinical variants include comedonal acne, acne papulopustulosa or pustulosa, and acne cystica.
Comedonal acne
It represents the mildest variant of acne, which presents with non-inflammatory open and closed comedones [Figure 1]. Comedones contain inspissated shed keratin. Open comedones, also known as blackheads, have a conspicuous dilated follicular opening that contains keratin, while in closed comedones, or whiteheads, the follicular opening is not visible. Treatment includes topical retinoids and manual comedone extraction.[4]

- Multiple open and closed comedones in an adolescent male.
Acne papulopustulosa
Inflammatory acne, specifically acne papulopustulosa, refers to the stage where acne lesions transition to a papulopustular state [Figure 2]. They vary in size from 1 mm to 5 mm. When the severity of the lesions increases, they can become nodulocystic. Treatment includes topical retinoids and topical antibacterials like benzyl peroxide – alone or in combination. Oral treatments include antibiotics with anti-inflammatory effects such as tetracyclines and macrolides, and isotretinoin.[5,6]
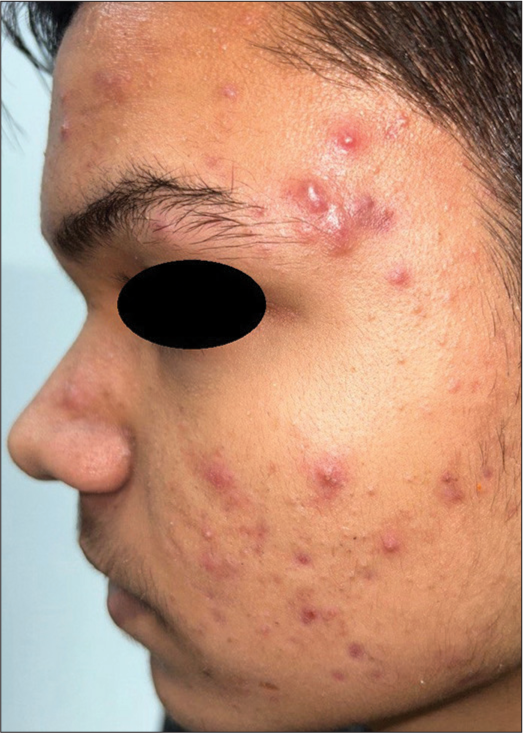
- Papulopustular acne in a 16-year-old male.
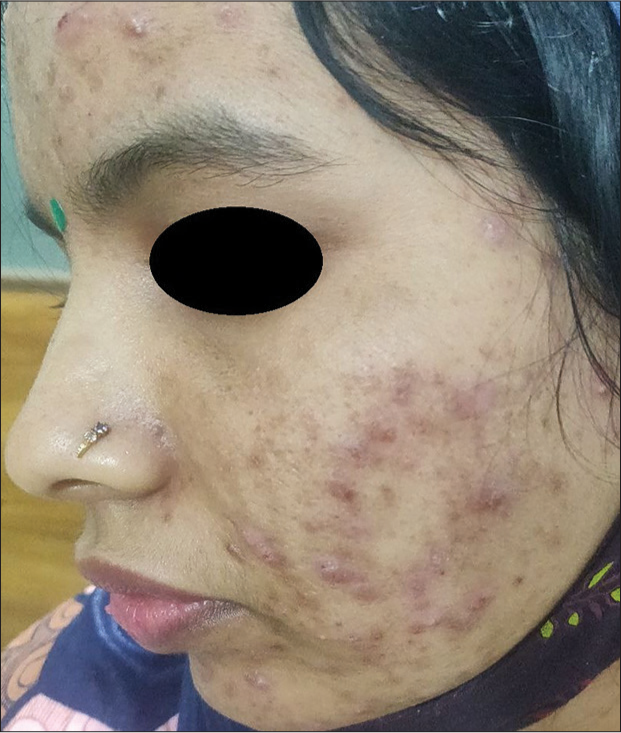
Acne cystica
This is also known as cystic or nodulocystic acne and presents as inflammatory cysts in severe acne vulgaris. As true cysts are uncommon in acne, they are called pseudocysts, which contain pus and some serosanguinous fluid [Figure 3]. Along with conventional anti-acne treatment including oral retinoids, these patients might require intralesional steroids. More severe variants include acne conglobata and acne fulminans.[5]

- Nodulocystic acne in a 19-year-old female.
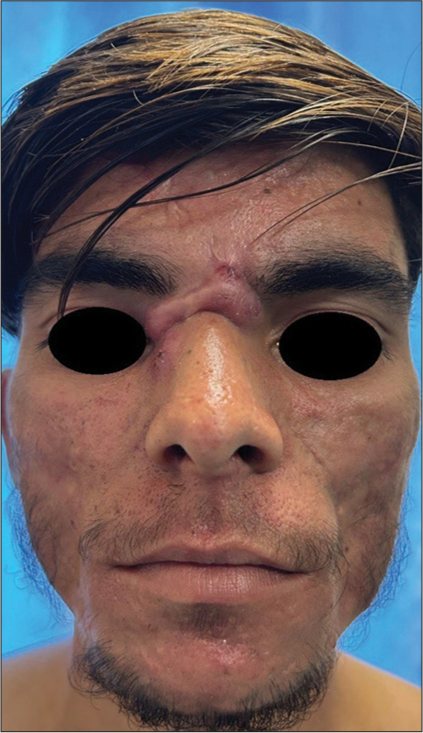
Acne conglobata
It is a severe form of cystic acne presenting as insidious onset extensive inflammatory papules, pustules, nodules, interconnecting abscesses, and sinus tracts in the background of multiple polyporous grouped comedones [Figure 4]. They heal with significant disfiguring scarring. Known associations include hidradenitis suppurativa (HS) and various follicular occlusion syndromes such as pyogenic arthritis, pyoderma gangrenosum, and acne (PAPA), pyoderma gangrenosum, acne, hidradenitis suppurativa (PASH), synovitis, acne, pustulosis, hyperostosis, osteitis (SAPHO), and pyoderma gangrenosum, acne conglobat, hidradenitis suppurativa, and seronegative spondyloarthritis (PASS). Treatment includes oral isotretinoin with or without oral steroids.[7]

- Acne conglobata in a young male.
Acne fulminans
It is also known as acne maligna or acute febrile ulcerative acne and presents as sudden onset tender ulceronecrotic nodulocystic lesions predominantly over the chest, upper back, shoulders followed by face [Figure 5], along with systemic symptoms such as fever, malaise, arthralgias, myalgias, osteolytic bony lesions of clavicle and sternum, and, rarely, hepatosplenomegaly, in patients with mild to moderate acne. They resolve with disfiguring severe scarring. Sudden onset and systemic symptoms distinguish it from acne conglobata. Association with SAPHO syndrome and PAPA is described in the literature. Treatment includes oral steroids followed by the introduction of oral isotretinoin at least after a month.[8]

- Acne fulminans in a 19-year-old male.
Isotretinoin-induced acne fulminans
Even though the treatment of acne fulminans includes systemic isotretinoin, rarely isotretinoin used in nodulocystic acne can precipitate acne fulminans with or without systemic symptoms. In the absence of systemic signs and symptoms, the condition is called “pseudo-acne fulminans” or “acne fulminans sine fulminans.” It is hypothesized to occur due to an exaggerated type III and/or type IV hypersensitivity response to the bacterial components of C. acnes, which are released following oral isotretinoin therapy. The resulting alterations in the immune system lead to variations in interleukin production and an intensified neutrophilic response resulting in the development of necrotizing ulcerative skin lesions.[9] Another hypothesis proposes that acne fulminans may occur due to a thinning of the follicular wall making it susceptible to rupture when exposed to isotretinoin. The release of follicular substances into the dermis triggers the recruitment of immune cells amplifying the immune response. In addition, prior use of topical steroids may exacerbate the thinning of follicular walls.[10] The flare usually occurs in the first month of therapy. Treatment includes oral steroids and lowering the dose or discontinuation of isotretinoin. Other systemic agents such as dapsone and clofazimine can also be used.[11]
Variants based on the age of onset
Pre-pubertal acne
Neonatal acne
It presents as inflamed papules and pustules over cheeks and nose, which begins around two weeks after birth and can last up to three months. Around 23–30% of cases exhibit the presence of comedones alongside facial pustules.[12] The pathogenesis involves Malassezia spp. along with the transient increase in sebum production after birth. They usually resolve spontaneously. However, topical ketoconazole can be used to hasten recovery.[13]
Infantile acne
It presents around three to six months of age and can last up to one to two years of life [Figure 6]. It has been attributed to the transient increase in androgen secretion (by the immature adrenals of the infant) and luteinizing hormone by the pituitary (stimulating testosterone production). Clinical presentations include both inflammatory and non-inflammatory lesions. Topical retinoids or benzoyl peroxide form the mainstay of treatment and are used as either monotherapy or in combination.[14]

- Infantile acne in a 4-month-old infant.
Mid-childhood acne
Clinicians should be watchful in children presenting with mid-childhood acne, as adrenarche is yet to be achieved and acne in childhood, especially between the ages of 1–7 years [Figure 7], should warrant the physician to look for endocrinological abnormalities causing hyperandrogenism. Detailed examination including a review of growth charts and secondary sexual characteristics is important to rule out hyperandrogenism. Treatment is similar to infantile acne.[13,14]

- Mid-childhood acne presenting over the forehead, dorsum of the nose, and left cheek in a 6-year-old boy.
Pre-adolescent
It presents between the ages of 7 and 12 years in boys or before menarche in girls, as predominantly comedones over the “T” area of the face (including the forehead and central face). Treatment is similar to adolescent acne, except that oral tetracyclines should be avoided in children <7 years.[13,14]
Adolescent acne
It presents between 12 and 19 years of age in boys or after menarche in girls. It is the most common age group for acne. The lesions can be both inflammatory and non-inflammatory.[13,14]
Post-adolescent acne/adult acne/adult-onset acne
Acne that presents in adults over the age of 25 years, either persistent or intermittent, is called adult acne.[15] It is more common in women and hence often called adult female acne. Adult female acne is further subdivided into two distinct categories: one for individuals aged 25–44 years and another for those aged over 45 years, particularly during the menopausal phase.[16]
Adult acne presents in three distinct forms:
Continuous or persistent: This is the most prevalent type and represents a continuation of acne from adolescence.
Late-Onset: Adult acne that appears for the first time during adulthood.
Recurrent: Adolescent acne, which temporarily improves but resurfaces again in adulthood.[17]
In addition, adult female acne has two clinical variants:
Inflammatory: Characterized by papules, pustules, and nodules on the lower one-third of the face, neck, and jawline, hence also called chin acne. Hyperseborrhea is not always a feature, and it is sometimes referred to as papulopustular post-adolescent acne.[16]
Retentional: Marked by numerous open comedones and microcysts across the entire face, with fewer inflammatory lesions. It consistently features hyperseborrhea and is also known as comedonal post-adolescent acne. This form can have a significant psychosocial impact, proving challenging to treat, and can become severe and disfiguring. It is linked to higher rates of smoking.[16]
Some of these women have other features of hyperandrogenism including polycystic ovary syndrome, hirsutism, and alopecia. Lesions can be both inflammatory and non-inflammatory. Treatment involves the use of conventional anti-acne agents in addition to anti-androgen therapies.[15]
Variants based on the body site involved
Truncal acne
It includes both inflammatory and non-inflammatory lesions of acne, involving the trunk, especially over the back and upper chest [Figure 8]. They usually have acne over the face simultaneously or in the past. It is treated on lines of acne vulgaris.[18]

- Truncal acne in an adult female.
Penile acne
Rarely, comedones, papules, pustules, and nodules can present over the proximal shaft of the penis [Figure 9] which responds to conventional anti-acne treatment.[19]

- Penile acne in a 21-year-old man.
Acne or post-acne scar
Post-acne scars can be atrophic, hypertrophic, keloidal or macular. Early treatment of acne is important in preventing this cosmetically disfiguring sequela of acne. Acne scars result from aberrant responses to different stages of wound healing, such as inflammation, granulation tissue formation, and extracellular matrix remodeling. Post-acne scars can be improved by various methods including, peeling, and lasers. It is the most common post-acne sequala, present in up to 90% of patients, in varying degrees.[20,21]
Acne scars can be divided into:
Atrophic acne scars
These are the most common types of acne scars, which are broadly classified into three types, namely, icepick, boxcar, and rolling scars [Figure 10a and b]. Icepick scars are the commonest, presenting as deep well-defined, narrow (<2 mm), scars that can extend up to deep dermis or subcutaneous tissue. Rolling scars are less demarcated atrophic scars with depth limited to the epidermis. They occur due to the tethering effect of fibrous scar in the dermis secondary to acne below a relatively uninvolved epidermis causing a shadowing/undulation. Boxcar or U-shaped scars are uniform, round, or oval scars with well-established vertical edges that reach a depth corresponding to the superficial or deep dermis and are usually wider at the surface.[20,21] Management of atrophic acne scars encompasses various treatment modalities, either alone or in combination, depending on the extent, severity, and type of acne scars. It includes topical retinoids, ablative lasers, chemical reconstruction of skin scars using trichloroacetic acid, fillers, microneedling, subcision, and excision.

- Atrophic acne scars (a) predominantly ice-pick with boxcar scars in a 24-year-old male (b) ice-pick, boxcar, and rolling scars in a 20-year-old female.
Macular acne scars
They present as erythematous, hypo- or hyperpigmented macules that occur secondary to inflammation or alteration in melanogenesis during different stages of wound healing [Figure 11].[20,21] Management includes topical retinoids, chemical peeling, and topical depigmenting agents.
- Macular acne scars in a 24-year-old female with active papulopustular acne.
Hypertrophic acne scars
They present as raised scars that remain within the boundaries of the initial acne lesion.[20,21] They occur due to excess collagen deposition and decreased collagen degradation. Management includes intralesional steroids or excision.
Keloidal acne scars
It present as raised scars that extends beyond the original boundaries of the lesions in individuals with keloidal tendency. Both hypertrophic and keloidal acne scars are more common on the trunk but may rarely occur over the mandibular area [Figure 12].[20,21] Management includes intralesional steroids, either alone or in combination with 5-fluorouracil and hyaluronidase.
- Keloidal acne scar over the root of the nose in a 28-year-old male.
Acne associated with other diseases
Acne can sometimes be a manifestation of endocrine abnormalities or a part of genetic or other syndromes. Often unusual presentation in terms of age, severity, type of lesions, and other supportive features point toward such a diagnosis.
Endocrine acne
It includes a spectrum of diseases with a similar pathology involving dysregulation of androgenic steroids, insulin resistance, and increased growth factor receptor signaling. This includes polycystic ovary syndrome [Figure 13], Cushing’s disease, late-onset congenital adrenal hyperplasia, seborrhea, acne, hirsutism, and alopecia (SAHA) syndrome, and hyperandrogenism, insulin resistance, and acanthosis nigricans (HAIR-AN) syndrome. These conditions either predispose or worsen acne vulgaris. This is also called hormonal acne and typically presents around the “U” area of the face. Treatment includes management of endocrine abnormality in addition to anti-acne therapies.[16]

- Endocrine/Hormonal acne with hirsutism in a 22-year-old female with polycystic ovarian syndrome.
Acne-associated auto-inflammatory syndromes
Acne can be an association of many syndromes including polygenic auto-inflammatory disorders. Overactivation of innate immunity leads to overproduction of Interleukin-1 (IL-1) family cytokines resulting in sterile neutrophil-rich cutaneous inflammation. Mutations affecting the structural proteins and functional proteins of the inflammasome complex have been observed in these disorders.[22] It includes:
PAPA: Pyogenic arthritis, pyoderma gangrenosum, and acne
PASH: Pyoderma gangrenosum, acne, and suppurative hidradenitis (HS) [Figure 14a-c]
PAPASH: Pyogenic arthritis, pyoderma gangrenosum, acne, and suppurative hidradenitis (HS)
PsAPASH: Psoriatic arthritis, pyoderma gangrenosum, acne, and suppurative hidradenitis (HS)
SAPHO: Synovitis, acne, pustulosis, hyperostosis, and osteitis
PASS: Pyoderma gangrenosum, acne conglobata, suppurative hidradenitis (HS), and seronegative spondyloarthritis.[22]

- Pyoderma gangrenosum, acne, hidradenitis suppurativa syndrome presenting in a 34-year-old male with (a) pyoderma gangrenosum-like ulcers over the left forearm, (b) papulopustular acne on the forehead, and (c) hidradenitis suppurativa over the right axilla.
Treatment includes conventional immunosuppressive agents and biologics. However, as these conditions are characterized by the overproduction of cytokines such as IL-1 and tumor necrosis factor alpha, biologics are considered superior to conventional immunosuppressants.
Acne associated with Apert syndrome
It is also known as acrocephalosyndactyly and is an autosomal dominant disorder that occurs due to a mutation in the FGFR2 gene. It presents with synostoses of cranium, vertebral bodies, hands, and feet.[23] They can present with comedones, papules, pustules, nodules, and cysts involving predominantly trunk and proximal limbs, sometimes extending to the dorsum of hands, in the background of severe seborrhea.[23,24] There are cases of acne in Apert syndrome successfully controlled with oral retinoids.[24]
Munro’s acne nevus: It is a mosaic cutaneous manifestation of Apert syndrome and occurs due to somatic FGFR2 mutation. It presents as comedones and inflammatory cysts arranged linearly along the lines of Blaschko.[23,24]
Other variants of acne
Acne excoriée
It is also known as excoriated or picker’s acne and is considered a psychodermatological disorder where often an adolescent female picks real or imagined acne lesions over the face out of compulsion or stress.[5] The presence of linear erosions is suggestive of self-inflicted disease, and it heals with significant scarring [Figure 15]. Unlike other psychodermatological disorders, the patient often readily accepts the skin-picking behavior.[5] In addition to skin-directed treatment, patients might require pharmacological and non-pharmacological psychiatric interventions. The latter includes hypnotherapy, habit reversal or cognitive behavioral therapy.[25-27]

- Acne excoriée over the nose in a 23-year-old female.
Granulomatous acne
It presents as well-demarcated deep nodules, especially over the cheeks. The pathogenesis is unknown at present. The response to oral antibiotics and isotretinoin is poor, often requiring oral steroids for management.[5]
Mechanical acne
Acne mechanica occurs due to obstruction of the pilosebaceous unit following repeated mechanical trauma in the form of pressure, friction or rubbing, which presents as comedones. The location varies with the area over which the pressure is applied, for example, in people who wear tight clothing, it happens around the straps, belts, headbands, and collars.[28] In violin players, it develops at the neck and over the back in truck drivers.[5] The clinical features include microcomedones and rarely secondary inflammatory papulonodules. Management includes prevention of the inciting mechanical trigger along with topical anti-acne treatment.
Many clinical variants of mechanical acne depending on the mode of mechanical injury and occupation are known. These include
Comb and brush acne: It occurs secondary to the repeated combing of hair. Decreased frequency of combing usually leads to the resolution of signs and symptoms.[29]
Stump acne: Acne-like lesions appear around the amputation stump secondary to mechanical friction from the prosthesis. The skin lesions can become severe, which could limit the mobility in these patients.[30]
Maskne: Mask-related acne occurs due to prolonged use of mask, which results in friction between the skin and mask textile. Mask usage increases the local temperature, modifying the skin microbiota and sebum production. It can present as new-onset acne or aggravation of preexisting acne localized to the area of the mask or perioral region (“O” area) [Figure 16].[31]

- Maskne presenting over the “O” area of the face around the nose and mouth, covered by the mask in a 21-year-old female.
Drug-induced acne
Acneiform eruptions, which are drug induced are often characterized by monomorphic inflammatory and non-inflammatory papules and nodules without any comedones [Figure 17]. The chest, upper back, and proximal upper limbs are the most common sites of involvement. Commonly implicated drugs include corticosteroids (through any route of administration- topical, oral, inhaled), anabolic steroids, anti-tubercular drugs (isoniazid and pyrazinamide), anti-retroviral drugs (ritonavir), mood stabilizers (lithium), contraceptives containing progestins, multivitamins (B2, B3, and B12), and epidermal growth factor receptor inhibitors.[32] Conventional anti-acne treatment usually leads to clinical improvement.

- Drug-induced acneiform eruption in a 28-year-old male secondary to anti-tubercular drug presenting as monomorphic erythematous follicular papules over lower back.
Acneiform eruption is the most common presentation of toxicity due to iodine (or for that matter any halogens, known as iododerma (halogenoderma). These are predominantly present over the seborrheic areas. It can present secondary to both oral and topical iodine preparations including oral and intravenous iodinated contrast dyes, drugs such as amiodarone, potassium iodide, and topical povidone iodine. Treatment includes excretion of iodine and avoiding further exposure.[33]
Acne venenata
Acne venenata or contact acne occurs due to several products, which come in contact with the skin. It is also called acne artificialis.
The subtypes include:
Acne cosmetica
It occurs due to the use of cosmetics containing potentially comedogenic substances such as lanolin, petrolatum, lauryl alcohol, and oleic acid, which may occlude the pilosebaceous duct and lead to comedone formation. It commonly presents with closed comedones and can exacerbate pre-existing acne.[5]
Pomade acne
It refers to non-inflammatory acne lesions on the face secondary to the use of “pomade,” a greasy/waxy substance that is used for defrizzing curly hair, which can also occlude the pilosebaceous duct [Figure 18].[34]

- Pomade acne presenting over the forehead in a 25-year-old male.
Detergent acne
Alkaline soaps and trauma secondary to frequent rough washing of the face can exacerbate pre-existing acne with predominant inflammatory lesions.[5]
Oil/tar/pitch acne
Oil, tar, and pitch are comedogenic, as they can clog the pilosebaceous ducts and hence produce acne in workers employed in tarring roads, roofs, etc. As coal tar is also phototoxic, it can cause severe acne in photo-exposed areas, especially malar areas.[5] Pitch tar has been associated with the presence of acne lesions, predominantly comedones in the periorbital area.[35] Cutting oil/petroleum acne presents in places where the oil can easily spill or splash such as the face, forearms, and thighs.
Chapstick acne
It occurs secondary to repeated use of chapsticks/vaseline to hydrate the lips, there are reports of development of acne lesions in the form of a single row of large, open comedones along the entire cutaneous margin of the upper lip.[36]
Management of acne venenata includes avoidance of the incriminating agent, in addition to topical and/or oral retinoids with or without benzoyl peroxide.[5]
Occupational or environmental acne
Occupation-related acne is called occupational acne. Many etiological agents including polyhydrogenated hydrocarbons, coal tar and its products, petrol, and other physical, chemical, and environmental agents may play a role in its pathogenesis. In this context, many forms of acne venenata including oil, tar, pitch, cutting oil, and petroleum oil acne are occupational acne. The different types of occupational acne are as follows.
Chloracne
It presents with comedones, papules, pustules, and cysts, often resolving with scars, and decreased sebum production leading to gradual xerosis. The cyst content is usually straw colored. Patients are usually middle-aged adults, who are not acne prone.[5,37] A history of exposure to polyhalogenated organic compounds, also known as chloracnegens, is a must for the diagnosis. Dioxin is the most common and potent chloracnegen known. Toxins, especially dioxin can accumulate in the sebaceous glands and activate the aryl hydrocarbon receptor present on keratinocytes and sebocytes. On activation, they accelerate proliferation and terminal differentiation in keratinocytes while sebocytes are switched toward keratinocyte differentiation. This results in comedo formation and eventual atrophy of the sebaceous glands. Dioxin can act as an endocrine-disrupting compound by mimicking endogenous hormones like androgens, which further potentiates acne formation.[38] Histopathologically, they show characteristic epidermal and follicular hyperplasia with involuted sebaceous glands, distinguishing it from regular acne vulgaris. Treatment includes the elimination of chloracnegens through chelating substances such as synthetic dietary fat substitutes and long-term topical application of tretinoin.[37]
Tropical acne
It is also known as hydration acne and presents with severe exacerbation of pre-existing acne over the back, upper arms, buttocks, and thighs, on exposure to hot and humid climates. Pathogenesis is unknown at present; however, secondary infection with coagulase-positive Staphylococcus is usually present. Oral antibiotics can be helpful; however, relocating the patient to a cooler environment is more important.[39]
Radiation acne
Ionizing radiations as well as non-ionizing radiations such as ultraviolet- and infrared light can induce acneiform eruption. With ionizing radiations, the comedonal lesions and papules are restricted to the sites of radiation therapy, predominantly in the form of comedones and rarely inflammatory lesions, usually presenting weeks to months after the radiation therapy.[40,41] The exact pathomechanism is unknown and is theoretically attributed to an alteration in sebum production and chronic follicular inflammation secondary to radiation. Extraction of these comedones is often difficult and sometimes resembles comedones of Favre-Racouchot syndrome.[42] Deep cobalt therapy, megavoltage therapy, as well as X-rays may result in development of acne. Management includes comedo extraction, topical retinoids, and benzoyl peroxide.[43]
ACNE-UNRELATED TERMS/MISNOMERS
Acne agminata
It is also known as LMDF. It is a granulomatous disease of the face presenting as persistent erythematous papules and nodules without any background skin changes, over the peri-oral, peri-orbital areas, and the cheeks [Figure 19]. They are usually treatment resistant and heal with significant scarring. Histology shows granulomatous tissue reaction with central caseation. Some authors consider it as a variant of rosacea; hence, the synonym “granulomatous rosacea,” while others consider it to be a tuberculid due to the histopathological features, but very often clinical and laboratory investigation yields no evidence of tuberculosis and the disease does not respond to anti-tubercular therapy like other tuberculids.[44] Hence, a new terminology has come into practice, i.e., facial idiopathic granulomas with regressive evolution (FIGURE), which has no connotation to the earlier believed tubercular pathology.[45] The management of this relatively uncommon entity is based on case series and reports. Overall, they show variable responses to topical tacrolimus, oral tetracylines, retinoids, and dapsone and with relatively good response to oral steroids.[45]

- Acne agminata presenting in a 42-year-old woman over the face.
Acne necrotica
It is also known as necrotizing lymphocytic folliculitis and presents as itchy or painful recurring papules, pustules, and nodules healing with variable degrees of scarring. The pathogenesis is incompletely understood. The early lesions include erythematous umbilicated follicular papules, which show superficial perifollicular lymphocytic infiltration on histology. This is followed by progression to necrosis of the upper pilosebaceous unit and the adjoining epidermis and dermis with a predominant neutrophilic infiltration. Two common subvariants are identified:
Acne necrotica miliaris
It is also known as scalp folliculitis or Propionibacterium folliculitis and presents as itchy pustules on the scalp, predominantly over the frontal hairline. It heals with cribriform atrophic scarring. Some authors attribute the pathogenesis to a reactionary inflammation against micro-organisms residing in the skin, such as Propionibacterium acnes, Staphylococcus aureus, Malassezia, and Demodex mites.[46]
Acne necrotica varioliformis
It is usually distributed over the face, scalp, and neck with a predilection for seborrheic areas. Starting as umbilicated papules, they progress to focal areas of necrosis and crusting, which eventually heal in weeks with typical varioliform scars. The pathogenesis is proposed to involve S. aureus and P. acnes, but their exact role is not known.[46]
Due to the scarcity of literature about these entities, management is based on case series and case reports and includes topical metronidazole, ivermectin, oral macrolides, tetracyclines, retinoids, and dapsone, with variable success.[46]
Acne aestivalis
It is also known as actinic folliculitis, actinic superficial folliculitis, acne Mallorca or Goa acne. It is a rare photodermatosis thought to be caused by ultraviolet A radiation, presenting as folliculocentric monomorphic papulopustules over the photoexposed areas including the face, neck, upper chest, and back, with a latency period spanning from a few hours to days after sun exposure. Photoprovocation testing is diagnostic. The mainstay of treatment is photoprotection. Conventional anti-acne treatment is not useful.[47]
Acne keloidalis nuchae
More appropriately termed folliculitis keloidalis, it is a follicular inflammatory process of unknown etiology presenting as papulopustules over the nape of the neck but can extend upwards onto the scalp [Figure 20]. They progress to form hypertrophic scars (not a keloid), which fuse to become horizontal bands with many patients showing signs of persistent inflammation in the form of abscesses and discharging sinuses. Treatment includes topical/intralesional steroids, but the response may be suboptimal. Laser-assisted hair removal and surgical excision followed by secondary intention healing have been tried successfully.[48]

- Acne keloidalis nuchae presenting as a large hypertrophic scar with tufted hair over the nape of neck and occipital scalp in a middle-aged man.
Pseudoacne of the nasal crease
Pseudoacne of the nasal crease is a distinct condition characterized by acne-like lesions at the convergence of the middle and lower thirds of the nose, also referred to as the nasal crease, which corresponds anatomically to the point where the alar and triangular nasal cartilages meet. It has diverse clinical presentations including hypo- or hyperpigmented lines with or without atrophy along with milia, comedones, papules, pustules, nodules or firm white scars. Transverse nasal milia are considered a variant of this condition and are characterized by the predominance of miliary cysts. A number of these patients have a background of allergic rhinitis. The formation of this crease is linked to the repetitive upward rubbing of the nose in children experiencing symptomatic allergic rhinitis and itching. It was termed “pseudoacne,” as it may be mistaken for acne vulgaris. However, history and progression distinguish it from typical acne vulgaris, as it occurs in preadolescence and solely affects the nasal crease. Benzoyl peroxide or topical antibiotics may be used for inflammatory papules and pustules. Extirpation is required for milia. Surgical excision is used for substantial and persistent papules when medical interventions prove ineffective.[49]
Acne inversa
It is commonly known as hidradenitis suppurativa (HS) and is characterized by the presence of polyporous comedones, nodules, interconnecting abscesses, and sinus tracts, which heals with scarring over the intertriginous areas such as axilla, groin, gluteal cleft, and inframammary areas [Figure 21]. There is an association with acne conglobata/nodulocystic acne in patients of HS. Other associations include hyperandrogenism and obesity. The pathogenesis seems to be multifactorial. Keratinous occlusion of the hair follicle followed by swelling and rupture of follicles and inciting severe inflammation to its contents and aberrant immune response to skin commensals in genetically predisposed individuals are proposed pathomechanisms. Treatment includes long-term oral antibiotics and surgical interventions.[50]

- Acne inversa (hidradenitis suppurativa) presenting in a 27-year-old female.
CONCLUSION
The term “acne” has wide usage in dermatology, often leading to confusion between acne-related and -unrelated entities. This article attempts to summarize all such terms and provide readers with a ready reckoner for this complex lexicon.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- The origin and use of the word “acne”. Br J Dermatol. 1977;96:291-4.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of Shalmalyadilepa and Guduchyadivati in the management of Yauvanapidika (Acne) Ayu. 2013;34:174-9.
- [CrossRef] [PubMed] [Google Scholar]
- Comedone formation: Etiology, clinical presentation, and treatment. Clin Dermatol. 2004;22:367-74.
- [CrossRef] [PubMed] [Google Scholar]
- Acne In: Griffiths C, Barker J, Bleiker T, Chalmers R, Creamer D, eds. Rook's textbook of dermatology (9th ed). United States: Wiley-Blackwell; 2016. p. :90.1-65.
- [Google Scholar]
- Acne management guidelines by the dermatological society of Singapore. J Clin Aesthet Dermatol. 2019;12:34-50.
- [Google Scholar]
- Acne fulminans: Case Series and review of the literature. Pediatr Dermatol. 2016;33:e388-92.
- [CrossRef] [PubMed] [Google Scholar]
- Acne fulminans successfully treated with prednisone and dapsone. An Bras Dermatol. 2012;87:612-4.
- [CrossRef] [PubMed] [Google Scholar]
- Pseudo acne fulminans: An under recognized entity. Indian Dermatol Online J. 2018;9:462-4.
- [CrossRef] [PubMed] [Google Scholar]
- Acne fulminans induced by a low dose isotretinoin: Case report and review of the literature. Dermatol Online J. 2020;26:13030.
- [CrossRef] [Google Scholar]
- Pustular lesions in the neonate: Focused diagnostic approach based on clinical clues. Indian J Dermatol Venereol Leprol. 2022;88:708-16.
- [CrossRef] [PubMed] [Google Scholar]
- Consensus on neonatal through preadolescent acne. J Drugs Dermatol. 2020;19:592-600.
- [CrossRef] [PubMed] [Google Scholar]
- Acne in the first three decades of life: An update of a disorder with profound implications for all decades of life. Dis Mon. 2021;67:101103.
- [CrossRef] [PubMed] [Google Scholar]
- Adult-onset acne: Prevalence, impact, and management challenges. Clin Cosmet Investig Dermatol. 2018;11:59-69.
- [CrossRef] [PubMed] [Google Scholar]
- Adult female acne: A guide to clinical practice. An Bras Dermatol. 2019;94:62-75.
- [CrossRef] [PubMed] [Google Scholar]
- Adult acne versus adolescent acne: A retrospective study of 1,167 patients. J Clin Aesthet Dermatol. 2018;11:21-5.
- [Google Scholar]
- Dermatoses of the male genitalia In: Griffiths C, Barker J, Bleiker T, eds. Rook's textbook of dermatology (9th ed). Oxford: Blackwell Science; 2016. p. :111.1-36.
- [CrossRef] [PubMed] [Google Scholar]
- Acne scarring-pathogenesis, evaluation, and treatment options. J Clin Aesthet Dermatol. 2017;10:12-23.
- [Google Scholar]
- Methods for the improvement of acne scars used in dermatology and cosmetology: A review. J Clin Med. 2022;11:2744.
- [CrossRef] [PubMed] [Google Scholar]
- Pronounced and early acne in Apert's syndrome: A case successfully treated with oral isotretinoin. Eur J Dermatol. 2002;12:496-8.
- [Google Scholar]
- Using hypnosis to facilitate resolution of psychogenic excoriations in acne excoriée. Am J Clin Hypn. 2004;46:239-45.
- [CrossRef] [PubMed] [Google Scholar]
- Acne excoriée--a case report of treatment using habit reversal. Clin Exp Dermatol. 1989;14:163-4.
- [CrossRef] [PubMed] [Google Scholar]
- Cognitive behavioral therapy as an adjuvant therapy in acne excoriée: A randomized controlled clinical trial. J Dermatolog Treat. 2022;33:782-8.
- [CrossRef] [PubMed] [Google Scholar]
- Stump acne: A new variant of acne mechanica and a cause of immobility. Br J Dermatol. 2001;144:647-8.
- [CrossRef] [PubMed] [Google Scholar]
- Mask related acne ("maskne") and other facial dermatoses. BMJ. 2021;373:1304.
- [CrossRef] [PubMed] [Google Scholar]
- Drug-induced acneiform eruption. Am J Clin Dermatol. 2011;12:233-45.
- [CrossRef] [PubMed] [Google Scholar]
- An acneiform eruption secondary to iododerma. JAAD Case Rep. 2018;4:468-70.
- [CrossRef] [PubMed] [Google Scholar]
- Periorbital comedones and their relationship to pitch tar: A cross-sectional analysis and a review of the literature. J Am Acad Dermatol. 2000;42:624-7.
- [CrossRef] [PubMed] [Google Scholar]
- Environmental pollution and acne: Chloracne. Dermatoendocrinol. 2009;1:125-8.
- [CrossRef] [PubMed] [Google Scholar]
- Chloracne and hyperpigmentation caused by exposure to hazardous aryl hydrocarbon receptor ligands. Int J Environ Res Public Health. 2019;16:4864.
- [CrossRef] [PubMed] [Google Scholar]
- A severe form of acne developing in the tropics. Arch Derm Syphilol. 1949;60:206-16.
- [CrossRef] [PubMed] [Google Scholar]
- Acneiform eruption secondary to radiotherapy. Indian J Dermatol Venereol Leprol. 2021;87:587-8.
- [CrossRef] [PubMed] [Google Scholar]
- Comedogenic acne following radiation therapy. Eur J Dermatol. 2011;21:1017-8.
- [CrossRef] [PubMed] [Google Scholar]
- Favre-racouchot-like disease after radiation therapy. J Am Acad Dermatol. 2003;49:117-9.
- [CrossRef] [PubMed] [Google Scholar]
- Localized acne induced by radiation therapy. Dermatol Online J. 2014;20:21545.
- [CrossRef] [Google Scholar]
- Lupus miliaris disseminatus faciei. An Bras Dermatol. 2017;92:851-3.
- [CrossRef] [PubMed] [Google Scholar]
- Nosology and therapeutic options for lupus miliaris disseminatus faciei. J Dermatol. 2011;38:864-73.
- [CrossRef] [PubMed] [Google Scholar]
- Acne necrotica (necrotizing lymphocytic folliculitis): An enigmatic and under-recognised dermatosis. Australas J Dermatol. 2018;59:e53-8.
- [CrossRef] [PubMed] [Google Scholar]
- Other acquired disorders of the pilosebaceous unit In: Griffiths C, Barker J, Bleiker T, Chalmers R, Creamer D, eds. Rook's textbook of dermatology (9th ed). United States: Wiley-Blackwell; 2016. p. :93.1-32.
- [CrossRef] [Google Scholar]
- Treatment of acne keloidalis nuchae: A systematic review of the literature. Dermatol Ther (Heidelb). 2016;6:363-78.
- [CrossRef] [PubMed] [Google Scholar]
- Pseudoacne of the nasal crease: A new entity? Pediatr Dermatol. 2004;21:427-31.
- [CrossRef] [PubMed] [Google Scholar]





