Translate this page into:
Clinical and dermoscopic evaluation of red light emitting diodes with beta-carotene versus red light emitting diodes alone in treatment of photoaging

*Corresponding author: Tejinder Kaur, Department of Dermatology, Government Medical College, Amritsar, Punjab, India. tejinderkaurdr@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kumar M, Kaur T, Kaur I. Clinical and dermoscopic evaluation of red light emitting diodes with beta-carotene versus red light emitting diodes alone in treatment of photoaging. CosmoDerma 2023;3:32.
Abstract
Objectives:
Red light-emitting diodes (LEDs) alter the extracellular matrix and increase fibroblast growth factor which increases the number of fibroblasts. Carotenoids have singlet oxygen quenching properties. The objective of this study was to evaluate combined effect of red light with oral beta-carotene in treating photo-damaged skin.
Material and Methods:
Enrolled subjects were randomized into two groups, A and B. Group A received two sessions/week for 4 weeks of red light therapy and oral beta-carotene 30 mg/day for 12 weeks and Group B received two sessions/week for 4 weeks of red light therapy alone. Before and after clinical as well as dermoscopic photographs were evaluated. Dermoscopic photoaging scale (DPAS), Physician Global Assessment, and Patient Global Assessment was done at baseline, at end of therapy at 4 weeks and at 12 weeks.
Results:
The mean DPAS of Group A before the treatment was 22.76 which decreased to 10.08 at the end of follow-up period (12 weeks) and was 19.80 in Group B before the treatment which decreased to 10.84. There was 28.25% reduction in DPAS in Group A at 4 weeks whereas it was 16.18% in Group B. Group A showed 56.12% reduction at week 12, while Group B showed 44.78% reduction. There was statistically significant difference in mean percentage reduction in DPAS between the two groups when compared (P = 0.001).
Conclusion:
Red LED therapy with oral beta-carotene is a better approach for treating photoaging than Red LED therapy alone.
Keywords
Photoaging
Dermoscopy
Light emitting diodes
Beta-carotene
Phototherapy
INTRODUCTION
Photoaging refers to all the skin changes produced by chronic exposure to ultraviolet radiations which fall in the 290–400 nm wavelength spectrum. Cumulative exposure to solar radiation and interplay of various other factors such as genetic predisposition, geographical location, dietary habits, and lifestyle tend to cause complex skin alterations which can result in premature skin aging. Photoaging can manifest in the form of coarse wrinkles, fine lines, pigmentation, lentigines, roughness, rhytides, and telangiectasia which can overlay physiologically aging skin.[1] Apart from being a cosmetic concern, photoaging also poses a great risk of the development of cutaneous carcinomas as ultraviolet radiations also alter signal transduction pathways and cause DNA alterations. Hence, photodamaged skin is more prone to photocarcinogenesis.[2]
Photoaging is more commonly seen in fairer skin, Fitzpatrick I, II, and III and is less common in darker skin types, Fitzpatrick IV, V, and VI. Males tend to be more prone to photoaging and photo-carcinogenesis due to lack of photo-protective practices, more outdoor work, and decreased innate free radical scavenging activity. Female sex hormones are known to protect against photoaging. There is a greater tendency of wrinkling seen in females after menopause because of decreased estrogen levels.[3]
Light-emitting diode (LED) devices utilizing different wavelengths have many advantages that include rapid wound healing, acne and rosacea treatment, hair restoration, and skin photomodulation. Red LEDs alter the extracellular matrix by increasing matrix metalloproteinase-9 (MMP-9), and decreasing MMP-1, thus increasing procollagen-1. There is also an increase in fibroblast growth factor which increases the number of fibroblasts and histologically a mild inflammatory infiltrate following irradiation is seen. Red LEDs target dermal structures, such as adnexa and fibroblasts as it has the deepest tissue penetration among all the wavelengths in the visible spectrum.[4]
Skin naturally has an array of beneficial antioxidants which include endogenous enzymes such as glutathione (GSH) peroxidase, superoxide dismutase, catalase, and vitamin and minerals involved in biochemical reactions occurring in the body like Vitamin E and Vitamin C. A variety of natural antioxidants are derived from fruit and vegetable components. Non-vitamin plant-derived ingredients like soya also have a protective role. Beta-carotene is one of the provitamins which has a role in preventing and treating acute and chronic alterations produced by photodamage.[5]
Both red LEDs and beta-carotene have been studied extensively as individual modalities for treating photoaging. This study was taken up to evaluate the efficacy of the combination of red LED therapy and beta-carotene supplementation in the treatment of photoaging.
Changes in the photoaged skin occur at histological and biochemical levels which require biopsy as a part of the evaluation process which is invasive and undesirable by the patient. Dermoscopy can be used to examine the changes which cannot be seen with the naked eye and patients also tend to readily volunteer for examination as it is non-invasive. Therefore to study the efficacy of treatment modalities dermoscopic photoaging assessment was done.
MATERIAL AND METHODS
Participants
Fifty patients consisting of men and women aged 35–65 years, with skin phototype II, III, IV, and V on Fitzpatrick scale and signs of aging II, III, and IV on Glogau scale were enrolled from the outpatient department of a tertiary center after taking the approval from the Institutional Ethics Committee. They were randomized into two groups, A and B comprising of 25 patients each. Group A received two sessions/week for 4 weeks of red light therapy and oral beta-carotene 30 mg/day for 12 weeks and Group B received two sessions/week for 4 weeks of red light therapy alone [Figure 1]. All subjects provided written informed consent to participate in the study.

- Study design flowchart.
Exclusion criteria
The exclusion criteria were: Presence of any active infection or photodermatoses, active rosacea, active inflammatory dermatoses (atopic dermatitis, psoriasis), history of any photosensitizing drug usage, patients on immunosuppressive therapy, and utilization of any kind of topical treatment (e.g., Topical retinoid, azelaic acid creams, and topical steroids) in the previous 1 month, surgical esthetic treatment in the previous 6 months and local injection therapies or cosmetic procedures in the previous 6 months.
Equipment
The light source was LED (O’melon Omega Led) system containing 283 units (in three panel) that emit red light, with 640 nm wavelength and delivered an irradiance of 0.47 mW/cm2, and fluence of 0.84 J/cm2 [Figure 2]. For dermoscopic assessment of the face AM7515MZT Dino-Lite Edge Videodermoscope (Taiwan) with ×60 magnification in polarized mode was used [Figure 3]. Capsule Oxidon Plus (Micro labs limited) containing 30 mg beta – carotene was given to patients in Group A.

- Light-emitting diode system.

- Assessment of the face AM7515MZT Dino-Lite Edge Videodermoscope.
Procedure
At the beginning of the study, patient with photodamaged skin was enrolled after clinical and baseline assessment. Dermoscopic examination of all the cases was done.
Patients were classified according to the Glogau Scale into Group I, Group II, Group III, and Group IV.[6] Physician global assessment (PhGA) was done through a 5-point scale (score ranging from 0 to 4) for seven skin features of photodamage which included global score, fine lines, mottled pigmentation, sallow complexion, tactile roughness, telangiectasia, and coarse wrinkles. Baseline dermoscopic evaluation of the photo-damaged skin was done. Skin was assessed on the basis of Dermoscopic Photoaging Scale (DPAS) consisting of 11 features of photo-damage assessed over four areas of the face (forehead, right cheek, left cheek, and chin). It involved yes (1) or no (0) policy with score ranging from 0 to 11 for one area of face and total score of the face ranging from 0 to 44[7] [Table 1].
| Criteria | Forehead | Right cheek | Left cheek | Chin |
|---|---|---|---|---|
| Yellowish discoloration | 0/1 | 0/1 | 0/1 | 0/1 |
| White line | 0/1 | 0/1 | 0/1 | 0/1 |
| Lentigo | 0/1 | 0/1 | 0/1 | 0/1 |
| Hypo-hyperpigmented macules | 0/1 | 0/1 | 0/1 | 0/1 |
| Telangiectases | 0/1 | 0/1 | 0/1 | 0/1 |
| Yellowish papules | 0/1 | 0/1 | 0/1 | 0/1 |
| Actinic keratosis | 0/1 | 0/1 | 0/1 | 0/1 |
| Senile comedones | 0/1 | 0/1 | 0/1 | 0/1 |
| Deep wrinkles | 0/1 | 0/1 | 0/1 | 0/1 |
| Superficial wrinkles | 0/1 | 0/1 | 0/1 | 0/1 |
| Criss cross wrinkles | 0/1 | 0/1 | 0/1 | 0/1 |
| Total score | 0-11 | 0-11 | 0-11 | 0-11 |
| 0-44 | ||||
After gentle cleansing face was irradiated with red LEDs for a total period of 20 min. Patients were advised to apply sunscreen and emollients over both sides after the procedure. The subjects were instructed to follow photoprotective measures. Sun protection with sunscreen was advised at the start of therapy, during the treatment and in follow-up period. The procedure was done up to 8 times, two sessions/week over a period of 4 weeks. Group A received daily oral beta-carotene 30 mg for 3 months along with red light therapy while Group B received only red light therapy. Assessment was done at baseline, end of red light therapy (4th week) and at 12th week. To assess the clinical response, photographic documentation of all the patients was done with identical camera settings, illumination and from a fixed distance. Frontal, right, and left views for each patient were photographed. PhGA (ranging from 0 to 21), patient global assessment (PGA) (ranging from 0 to 10), and dermoscopic assessment was performed and any adverse events and complications were recorded. In PGA, patients were asked to score the improvement of on a visual analogue scale from 0 to 10 with 0 as no improvement and 10 as the best possible improvement.
The data were entered into Microsoft Excel spread sheet and results were analyzed using Statistical Package for the Social Sciences version 21. Mean and standard deviation were calculated for continuous parameters. Quantitative variables were compared using unpaired t-test between two groups. Qualitative variables were correlated using Chi-square test and correlation analysis. P < 0.05 was considered statistically significant.
RESULTS
Patient demographics
Fifty subjects were enrolled and completed the study. Both Group A and B comprised of 25 patients each. There was no significant difference in the demographic data between the two groups [Table 2].
| Demographic Data | Demographic data | Group A (n=25) (%) | Group B (n=25) (%) | P-value |
|---|---|---|---|---|
| Gender | Female | 24 (96) | 24 (96) | 1.000 |
| Male | 1 (4) | 1 (4) | ||
| Age | 35–45 | 2 (8) | 1 (4) | 1.381 |
| 45–55 | 12 (48) | 16 (64) | ||
| 55–65 | 7 (28) | 5 (20) | ||
| 65–75 | 4 (16) | 3 (12) | ||
| Occupation | Housewife | 16 (64) | 10 (40) | 4.689 |
| Teacher | 3 (12) | 2 (8) | ||
| Nursing staff | 4 (16) | 7 (28) | ||
| Service | 2 (8) | 6 (24) | ||
| Marital Status | Married | 25 (100) | 21 (84) | 0.110 |
| Unmarried | 0 (0) | 4 (16) | ||
| Precipitating Factors | Family history | 7 (28) | 9 (36) | 0.762 |
| Use of cosmetics | 11 (44) | 5 (20) | 0.128 | |
| Use of home remedies/any oil etc | 10 (40) | 7 (28) | 0.551 | |
| Drugs | 11 (44) | 13 (52) | 0.776 | |
| Co morbid illness | 7 (28) | 832) | 7.029 | |
| Extent of sun exposure | None or mild | 0 | 0 | 1.786 |
| Moderate | 14 (56) | 18 (72) | ||
| Severe | 8 (32) | 6 (24) | ||
| Very severe | 3 (12) | 1 (4) | ||
| Fitzpatrick Skin Type | III | 17 (68) | 14 (56) | 0.983 |
| IV | 5 (20) | 8 (32) | ||
| V | 3 (12) | 3 (12) | ||
| Glogau Group | I | 0 (0) | 0 (0) | 0.567 |
| II | 9 (36) | 12 (48) | ||
| III | 16 (64) | 13 (52) |
Primary outcome: Dermoscopic photoaging score (DPAS) and PhGA
Three blinded evaluators evaluated the mean DPAS of four areas of face, forehead, right cheek, left cheek, and chin. On baseline dermoscopic examination, most consistent findings were yellowish discoloration, hypohyperpigmented macules, and superficial wrinkles seen in all patients, that is, 50 (100%) of the study cases followed by yellowish papules seen in 48 (96%), deep wrinkles 33 (66%), lentigo 32 (64%), telangiectasia 23 (46%), criss cross wrinkles 12 (24%), and white line 6 (12%) study cases. None of the patients in the study group had senile comedones and actinic keratosis [Figure 4].

- Baseline dermoscopic features seen in participants.
The mean DPAS of Group A before the treatment was 22.76 which decreased to 16.2 (P = 0.002) at 4th week and further decreased to 10.08 at the end of follow-up period (12 weeks). Significant reduction in DPAS in comparison to baseline value was noted (P = 0.000). The mean DPAS in Group B before the treatment was 19.80 which decreased to 16.68 (P = 0.000) at 4th week and further decreased to 10.84 at the end of follow-up period (12 weeks). Statistically significant reduction in DPAS in comparison to baseline value was noted (P = 0.004) [Table 3]. Representative before and after dermoscopic photographs of patients in Group A and Group B are shown in [Figures 5 and 6], respectively.
| Group | Duration | Mean DPAS | Standard Deviation | P-value |
|---|---|---|---|---|
| Group A | Baseline | 22.7600 | 4.711 | - |
| 4 weeks | 16.2000 | 4.528 | 0.002 | |
| 12 weeks | 10.0800 | 3.785 | 0.000 | |
| Group B | Baseline | 19.800 | 3.166 | - |
| 4 weeks | 16.680 | 3.010 | 0.000 | |
| 12 weeks | 10.840 | 1.772 | 0.004 |

- Representative before and after dermoscopic photographs of participants in Group A (×60 polarized mode).

- Representative before and after dermoscopic photographs of participants in Group B (×60 polarized mode).
The mean PhGA in Group A was 14.800 ± 3.582 at baseline and after 4 weeks of treatment, it decreased to 9.9200 ± 3.558 and at the end of follow-up period of 12 weeks, it was 7.0800 ± 3.135. The reduction in the score was statistically significant (P = 0.000). The mean PhGA in Group B was 14.040 ± 2.590 at baseline and after 4 weeks of treatment, it decreased to 10.520 ± 2.293 and at the end of follow up period of 12 weeks, it was 7.040 ± 2.169. The reduction in the score was statistically significant (P = 0.001) [Table 4]. Representative before and after photographs of patients in Group A and Group B are shown in [Figures 7 and 8], respectively.
| Group | Duration | Mean PhGA | Standard Deviation | P-value |
|---|---|---|---|---|
| Group A | Baseline | 14.800 | 3.582 | |
| 4 weeks | 9.9200 | 3.558 | 0.000 | |
| 12 weeks | 7.0800 | 3.135 | 0.000 | |
| Group B | Baseline | 14.040 | 2.590 | |
| 4 weeks | 10.520 | 2.293 | 0.000 | |
| 12 weeks | 7.040 | 2.169 | 0.001 |
PhGA: Physician global assessment

- Representative before and after dermoscopic photographs of participants in Group A.

- Representative before and after photographs of participant in Group B.
There was 28.25% reduction in DPAS in Group A at 4 weeks whereas reduction was 16.18 % in Group B. Group A showed 56.12 % reduction at week 12, while Group B showed 44.78 % reduction. There was statistically significant difference in mean percentage reduction in DPAS between the two groups when compared. (P = 0.001) [Figure 9].
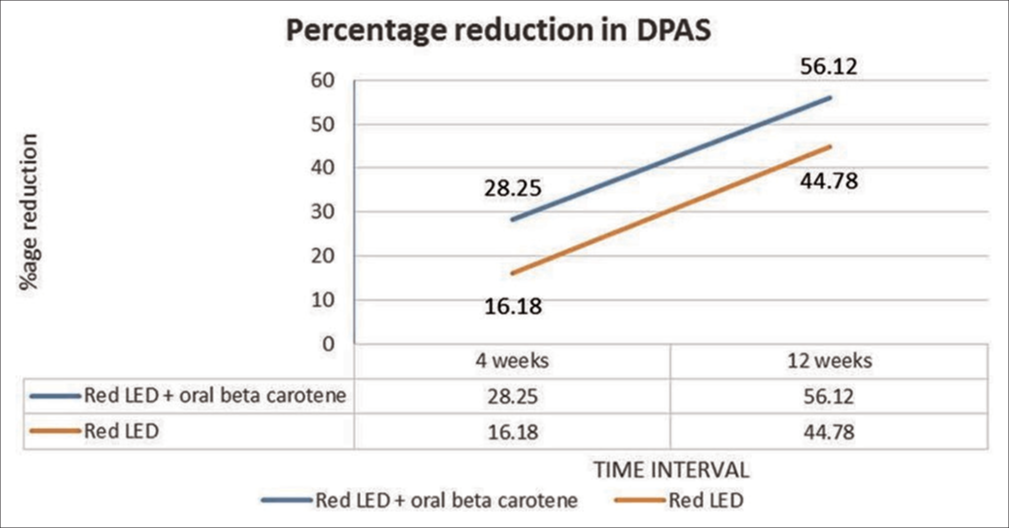
- Percentage reduction in DPAS in Group A and Group B.
Secondary outcome: PGA
The mean PGA in Group A was 5.125 ± 0.771 after 4 weeks of treatment which increased to 6.25 ± 1.083 at the end of follow-up period (12 weeks). The mean PGA in Group B was 5.000 ± 0.917 after 4 weeks of treatment which increased to 5.542 ± 1.292 at the end of follow-up period (12 weeks).
In Group A, 4 (16%) while in Group B, none of the study cases showed very good improvement (>75% reduction in DPAS). In Group A, 18 (72%) while in Group B, 9 (36%) of the study cases showed good improvement (50–75% reduction in DPAS). Moderate improvement (25–50% reduction in DPAS) was seen in 4 (16%) and 16 (64%) patients, in Groups A and B, respectively. Statistically significant difference in grades of therapeutic improvement was noted between both the groups (P = 0.001). In both the groups, no subject reported dissatisfaction at either 4- or 12-week follow-up [Figure 10].
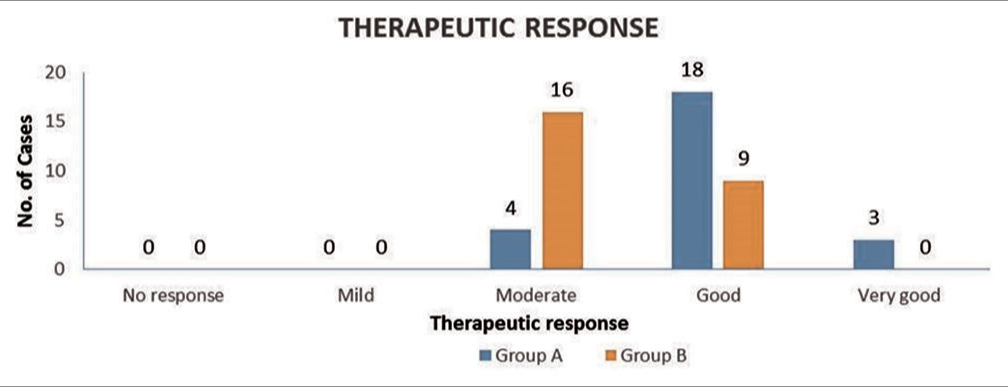
- Therapeutic response in Group A and Group B.
Safety outcome: Tolerability and adverse events
Erythema was the only complaint experienced by 2 (4%) cases, one in each Group A and Group B. However, this side effect subsided within 24–48 h period in both the patients.
DISCUSSION
Photoaging is the process of accelerated skin aging due to chronic solar exposure. Few of the signs are common to both photoaging and photo-protected chronologically aged skin. Photoaging causes significant psychological distress and frustration in the affected individuals due to considerable cosmetic disfigurement and remains a difficult condition to treat. Irradiation with red LEDs targets collagen and reduces the induction of MMP enzymes due to the fact, it can penetrate up to 6 mm of skin. Dietary substances such as beta-carotene, collagen peptides, zinc, and fat-soluble Vitamins D and E also have benefits in preventing and repairing photoaging. Beta-carotene is a plant-derived carotenoid that has a free radical scavenging action. The efficacy of light therapy with concomitant oral beta carotene supplementation has not been studied earlier. The quantitative assessment of efficacy of this combined modality can be studied through dermoscopic photoaging scale (DPAS).
The risk of wrinkling and pigmentary changes increases as such with age. People in their sixties are 12 times more prone to wrinkling, and subjects in their seventies are 56 times at a higher risk compared to the younger group. It is believed that pigmentary changes are more evident clinical signs of photoaging in Asians and that wrinkling is late compared to Caucasian subjects of a similar age.[8] However, we found that both wrinkling and pigmentary changes were a prominent feature of cutaneous photodamage in our patients and were seen at an early age of 35 years.
Intrinsic aging affects both genders equally while photoaging is seen more in males owing to greater duration of exposure to the sun. Females have increased skin thickness, moisture retention, and decreased skin wrinkling because of the protective effect of estrogen.[3] In our study, most of the patients were female, 48 (96%). This does not reflect the true epidemiology as female attendance for cosmetic issues is more. This fact is consistent with the previous studies where more female patients were enrolled.[9,10]
Occupation holds significance in regards to the degree of sun exposure. In a study conducted by Green et al., it was found that individuals who had outdoor occupations had 60% raised odds of higher grades of photoaging.[11] This was not consistent with our study as housewives who do not have much photo exposure constituted a majority i.e. 26 (52%) of our patients.
The role of cosmetics and intake of certain drugs such as photosensitizing substances have also been considered as risk factors for photoaging. Use of cosmetics and oil application was reported in 17 (34%) in the form of over-the-counter fairness cream, cold cream, bleaching creams, foundations, etc. These products when used for a long duration can lead to serious complications like epidermal thinning, atrophy, and can also make the skin photosensitive.[12]
History of intake of systemic drugs was reported in 10 (20%) study cases. The most common type was ayurvedic and homeopathic medication followed by thyroxine, antihypertensives, and other medications like analgesics.
It was found that hypothyroidism was the most common associated comorbidity. It was seen in five patients (three in Group A and two in Group B). There are studies that correlate the presence of subclinical hypothyroidism with increasing age. A study conducted by Bocheva et al. emphasizes that hypothyroid state could be a risk factor for increased oxidative skin damage in chronically photo-exposed skin due to oxidative stress. Lipid peroxidation is one of the main steps through which photo-oxidative stress helps in causing photocarcinogenesis and photoaging.[13]
Both groups showed significant reduction in DPAS at 4th and 12th week follow-up suggesting decrease in signs of photodamage. Majority of the patients reported improvement in skin smoothness, firmness, and complexion with softening of fine lines in both the groups. Tolerance of treatment was good in both the groups. However, there was 28.25% reduction in DPAS in Group A and 16.18% in Group B at 4 weeks. Group A showed 56.12% reduction and Group B showed 44.78% reduction at 12 weeks. While both the groups showed improvement, on comparing the two groups, it was seen that addition of oral beta-carotene in Group A along with red light therapy resulted in significant superior results than what was seen in Group B (red light therapy alone). Therefore, we suggest that combination red light therapy with oral beta-carotene is better, convenient, and effective approach than red light therapy alone in the treatment of photoaging.
Limitations of the study included small sample size. There is a possibility of observer’s bias as DPAS is a subjective assessment tool. A longer follow-up period could have allowed for assessment of the longevity of all the outcomes.
CONCLUSION
Our results suggest that red LED therapy with concomitant oral beta-carotene is effective in treatment of photoaging without significant adverse effects.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Mechanisms of photoaging and cutaneous photocarcinogenesis, and photoprotective strategies with phytochemicals. Antioxidants. 2015;4:248-68.
- [CrossRef] [PubMed] [Google Scholar]
- Photoaging: A review of current literature. Curr Dermatol Rep. 2020;9:22-9.
- [CrossRef] [Google Scholar]
- Light-emitting diodes: A brief review and clinical experience. J Clin Aesthet Dermatol. 2015;8:36-44.
- [Google Scholar]
- Skin photoaging and the role of antioxidants in its prevention. ISRN Dermatol. 2013;2013:930164.
- [CrossRef] [PubMed] [Google Scholar]
- Aging in elderly: Chronological versus photoaging. Indian J Dermatol. 2012;57:343-52.
- [CrossRef] [PubMed] [Google Scholar]
- Development of skin aging scale by using dermoscopy. Skin Res Technol. 2013;19:69-74.
- [CrossRef] [PubMed] [Google Scholar]
- Photoaging in Asians. Photodermatol Photoimmunol Photomed. 2003;19:109-21.
- [CrossRef] [PubMed] [Google Scholar]
- Fractionated carbon dioxide laser treatment of photoaging: Prospective study in 45 patients and review of the literature. Dermatol Surg. 2011;37:1279-90.
- [CrossRef] [PubMed] [Google Scholar]
- Application of a new intense pulsed light device in the treatment of photoaging skin in Asian patients. Dermatol Surg. 2008;34:1459-64.
- [CrossRef] [Google Scholar]
- Factors associated with premature skin aging (photoaging) before the age of 55: A population-based study. Dermatology. 2011;222:74-80.
- [CrossRef] [PubMed] [Google Scholar]
- Complications of chronic use of skin lightening cosmetics. Int J Dermatol. 2008;47:344-53.
- [CrossRef] [PubMed] [Google Scholar]
- Does hypothyroidism augment sun-induced skin damage? Redox Rep. 2018;23:180-7.
- [CrossRef] [PubMed] [Google Scholar]






